Alzheimer’s may be caused by a ‘dirty brain’ – and a commonly used drug could ‘clean’ your mind

New research shows that Alzheimer’s disease can be treated with a drug we’ve been using for decades.
Researchers have discovered that a certain drug used to induce labor in pregnant women also speeds up the system that removes waste products from the brain, a system that does not function properly in humans.
That’s why some call Alzheimer’s and other dementias “dirty brain” diseases. When the waste disposal system slows down, toxic waste builds up in the brain, packing and damaging healthy tissue.
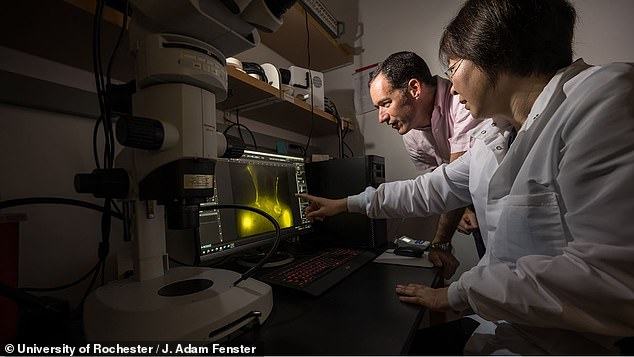
According to Dr. Douglas Kelley, a professor of mechanical engineering at the University of Rochester and leader of the study, administering drugs that cause muscle contractions can restore some of that function.
These drugs, which are used to help more than a million pregnancies worldwide each year, can be administered as a pill, intravenously or topically for $561.
The research, conducted at the University of Rochester by Dr. Douglas Kelley (left) and colleagues including Professor Tin Du (right), found that a commonly used drug could help restore glymphatic system function in older brains

The researchers examined the brain’s waste disposal system, called the glymphatic system, which slows down with age and in diseases such as Alzheimer’s and Parkinson’s.
‘“This study shows that restoring lymphatic function in the neck can significantly improve the slower removal of waste products from the brain that comes with aging,” said Dr. Kelley.
‘Furthermore, this was achieved with a drug that was already in clinical use, providing a potential treatment strategy.’
The study, which was published in the Nature Aging magazinelooked at the complex a series of tunnels and pumps that the brain uses to remove waste products, called the glymphatic system.
The system pumps fluid over the brain tissue, washing away old cells and proteins that can clog and damage neurons.
In a young, healthy brain, this system is well-oiled and efficient. But it slows down as we age or develop dementia.
One theory about Alzheimer’s is that this delay promotes the buildup of proteins called beta-amyloid.
Beta-amyloid is a naturally occurring protein that is processed in young brains when it is no longer useful and transported out of the body to be processed.
In Alzheimer’s, however, clumps of these dysfunctional proteins can build up, a hallmark of the disease, crowding out and killing healthy brain tissue.
A similar process occurs in Parkinson’s disease with another protein, namely alpha-synuclein.
Dr. Kelley was able to observe how waste processing in the brain slows down as mice age by marking the pumps in their brains and recording their functioning.
He found that in young, healthy mice, these pumps worked quickly, pumping a nearly constant flow of dirty fluid out of the brain.
In older mice, however, contractions were slowed by about 63 percent, allowing more “debris” to build up in the brain.
When the researchers saw this delayed pumping, they started thinking about a drug that has been used for years: prostanoids.
Prostanoids are medicines that affect prostaglandins, a type of fat that your body produces naturally and that, among other things, causes muscle contractions.
These drugs are useful in a wide range of medical situations, from inducing muscle contractions during labor to treating glaucoma and altering blood flow.
They were used to approximately 31 percent of American babies in 2020 – helping bring 1,117,612 new people into the world for approximately $561 per dose.
The best-known agent is misoprostol, one of the two drugs used in medical abortion.
The researchers applied a type of topical prostanoid medication to the necks of the mice, just above the pumps that process the brain’s waste. The theory was that this would help the muscles in the pumps turn on again.
The drug made the older mice’s pumps work faster again, making them as efficient as the young, healthy mice at removing old fluid from the brain.
“One can envision that this approach, possibly in combination with other interventions, could form the basis for future therapies for these diseases,” Dr. Kelley said.