DR. ELLIE: Can anything be done about my flatulence or do I have to learn to live with it?



I have been suffering from excessive flatulence for a while and it is very annoying – I feel like I have to go to the toilet all the time. Can anything be done about it? Or is it something I will have to live with?

Flatulence may be transient, but for some patients it is a medical condition
Dr. Ellie Cannon replies: Flatulence is of course normal. But if someone suffers from excessive flatulence, it can be very uncomfortable and socially embarrassing. So how much is normal? It’s difficult to pinpoint an exact number of times someone should ‘gas’, but a rule of thumb would be that if it happens significantly more often than someone is used to, it could be considered excessive.
Sometimes it is transient, caused by eating fiber-rich foods such as beans, legumes and vegetables. Intestinal bacteria help break these down and a byproduct of the process is gas.
But for some it is a medical condition. Irritable bowel syndrome can cause excessive bloating and flatulence, in addition to abdominal pain and diarrhea or constipation. Peppermint oil capsules can be given by prescription to reduce symptoms. Avoiding certain food groups under medical supervision can also help.
Excessive wind can also be caused by intestinal problems, including constipation, celiac disease and lactose intolerance. Less commonly diagnosed is a condition called small intestinal bacterial overgrowth (SIBO), in which excess bacteria build up in the intestines. Flatulence can be caused by a food intolerance. They are difficult to diagnose and rely on you keeping a meal diary to see which foods are linked to the problem. Some medications can cause excessive flatulence, such as statins and anti-inflammatories such as ibuprofen. Laxatives are also known to cause the problem.
I had a mini-stroke in my 50s and am taking ramipril, pravastatin and clopidogrel to prevent another stroke. Now my doctor wants me to take another medication, lansoprazole, to prevent stomach bleeding caused by the other medications. But if it’s the tablets that are causing the problem, can’t I take less?
Dr. Ellie answers: It is common that after a mini-stroke – also called a transient ischemic attack (TIA) – medications are prescribed to prevent another stroke. These are usually blood pressure tablets and a statin, to lower cholesterol, plus an blood thinner or anticoagulant medication.
Clopidogrel is one of them: it prevents certain cells in the blood – platelets – from clumping together and forming a clot. And it’s blood clots that travel to the brain that can cause TIAs.
However, one of the side effects of clopidogrel is bleeding. Stomach bleeding can happen to anyone, especially people with stomach irritation or stomach ulcers. The concern for someone taking clopidogrel is that this bleeding may become excessive and dangerous. Therefore if
If someone is taking an anticoagulant medication, something is often recommended to protect the stomach from irritation and possible bleeding. Lansoprazole is a medication that protects the stomach to make irritation or bleeding unlikely.
If clopidogrel works and doesn’t cause any problems, there is no reason to stop taking it. At the age of 77, the risk of a new TIA is greater than at the age of 57, purely because of age. So there would be no point in stopping clopidogrel unless it is causing problems.
I’m in my 80s and fit. But recently I noticed that after about 10 minutes of walking, my legs were numb and hard to control. My GP suggested it was due to nerve problems in my back and referred me for an x-ray. But I don’t have back pain. What do you think?
Dr. Ellie answers: Numbness and difficulty walking can be a neurological problem – conditions that affect the nerves. But symptoms like the ones you describe can also be related to a problem with blood circulation to the legs.
It’s called peripheral vascular disease and causes a very noticeable pain after walking that goes away when you rest. It can lead to aching pain in both legs and there may also be changes in skin color – the legs or feet may appear blue or purple – numbness or weakness. Peripheral vascular disease is more common in people who suffer from heart disease. And anyone with high blood pressure, obesity or high cholesterol is also at risk.
Smoking is the biggest cause. However, a doctor might consider this less likely in someone with a healthy lifestyle who reports these symptoms. Checking the pulse and blood pressure in the feet and legs can be done as an initial check to see if there is a vascular problem – this can be carried out at your local GP’s surgery. That said, numbness in the legs is also often caused by problems in the spine – and there may be no accompanying back pain.
The nerves that supply the legs are all connected to the spine, and any swelling or damage caused by conditions such as arthritis can lead to pressure on the spinal nerves.
This can then lead to numbness and possibly tingling, tingling or even weakness in the legs. It can only happen in certain positions, for example when you are walking and the pressure on the nerves is at its highest. It may stop when you move, sit or lie down and the pressure disappears.
Danger of slap-cheek syndrome

Parvovirus is known as ‘slapped cheek syndrome’
Have you heard of parvovirus? It is the cause of ‘slapped cheek syndrome’ in children – and despite the rash, is usually harmless.
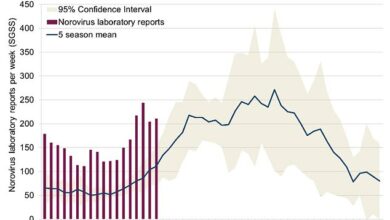
However, if a pregnant woman contracts the virus, it can lead to a miscarriage in one in eight cases. And worryingly, the number of women of childbearing age testing positive for parvovirus has skyrocketed since Covid.
I’ve heard stories of women losing babies due to the infection. We don’t have a vaccine right now, so it’s really something to be aware of.
I have never been shy about expressing my concerns about the endless lockdowns and the knock-on effects this would have on our health. Common infections were suppressed for years while we were isolated, and now seem to be circulating with a vengeance. I’m sorry to say that this seems to be another example.
How you can help our A&Es
The seemingly intractable problems with A&E are depressing. Wards are so overwhelmed with patients that hundreds of thousands are waiting more than 12 hours to be seen – in the most extreme case, according to recent data, they were waiting 10 days.
The situation is only getting worse and worse. Blame is often placed on GPs who cannot see patients quickly enough. In reality, people clog emergency services with things like mouth ulcers and coughs – things for which they really shouldn’t need medical attention.
A patient of mine who collapsed this week never made it to hospital – the emergency department was too busy so he was treated outside in the ambulance. Fortunately, that ended well.
Others haven’t been so lucky. I read about a disabled woman with severe asthma who died after waiting 39 hours in the emergency room.
How is your local hospital dealing with it? Write and let me know.
Do you have a question for Dr. Ellie Cannon? Email DrEllie@mailonsunday.co.uk
Dr. Cannon cannot enter into personal correspondence and her responses must be placed in a general context.