DR. MARTIN SCURR: Doctors like me can have a hard time when a patient asks how long he has to live (and why we all too often get the answer wrong)


What does having a terminal diagnosis mean? As a doctor I use the term, but I know that predicting what happens after such a diagnosis is virtually impossible.
I am currently caring for a patient who was expected to live for weeks because she has sarcoma (a form of cancer of the bone and soft tissue) that had already spread throughout her body when it was discovered.
She had no treatment: the decision was that chemotherapy would only make her sicker. Yet she remains active and independent two years after diagnosis.
I have a patient still alive, years after three recurrences of widespread malignant melanoma (a deadly form of skin cancer) – again, defying all predictions.
When I give advice to doctors training to become GPs, a constant theme is that none of us, no matter how experienced, can ever predict when a patient will die and that every doctor will have had patients who have overcome all odds.
A famous example was Abdelbaset al-Megrahi, the man convicted of the Lockerbie bombing who was diagnosed with aggressive prostate cancer in 2008 and released from prison on compassionate grounds in September 2009 because doctors believed he had only had a few months to live.
He survived for almost three years at home in Libya.

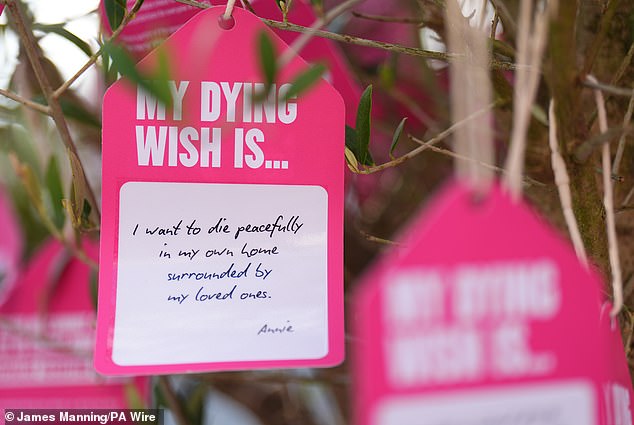
A ‘dying wish’ tied to a tree by a group of terminally ill people and bereaved people, in support of the Terminally Ill Adults (End of Life) Bill, in Parliament Square in London
Underestimating the time a patient has left may not sound like it’s a problem, but it is when it comes to discussions about assisted dying and whether it is something our society should allow. This will be subject to a free vote by MPs in the House of Commons on Friday, and last week Palliative Care Minister Stephen Kinnock became the first minister to publicly confirm he would vote in favor of passing the measure.
The question is about the prospect of helping those who want to end their lives to do so. This is not euthanasia – that is, giving someone the drug that kills them – but rather giving them the drugs to self-administer (as is the case with Dignitas, the clinic in Switzerland that makes doctor-assisted suicide possible).
My major concern as a primary care physician who has worked for many years as a hospice physician is that any new law will follow the model that has been allowed in Oregon, USA, for more than 20 years: if a patient is deemed to have less than six months of has time To stay alive, doctors can provide them with life-ending medications due to an incurable disease, which the patient can then administer themselves.
The problem is that research shows that doctors are often unable to accurately predict how long such patients will survive. A 2000 study in the BMJ of 343 patients found that doctors correctly predicted their life expectancy after hospice admission in only 20 percent of cases.
I am not against assisted dying, but against the way it is framed. I believe that rather than focusing on life expectancy, we should instead look at the level of disability. I think of people living with a condition that makes life unbearable – for example, robbing them of their ability to move or even swallow, and yet there is no clear point at which their distress could end.
Here I am thinking of conditions such as motor neurone disease, or strokes that affect both hemispheres of the brain, leaving a patient completely immobile; and yes, even those with an incurable disease who are entering a marked decline (which I think is an appropriate description of ‘terminal’).
Earlier this year, a patient I had been treating for years was diagnosed with incurable cancer, but no exact timetable was given for how long he had left. Within weeks he was bedridden and the only option was to reduce his pain. The support I offered was palliative care, an important part of which involves spending time with the patient, listening to their concerns and helping them come to terms with their death; the regret, the sadness, even the anger. Some patients find comfort and peace, but that is not the case everywhere. Despite the care I was able to provide, my patient suffered.

Dr. Martin Scurr says it is vital that we do not base any assisted dying law on an arbitrary guess about how much time a patient has left.
A fiercely independent man, he was devastated to suddenly find himself bedridden and unable to even lift a cup to have a drink. For over a month he became increasingly upset. Over and over again he begged me to get something to release him.
He died a while after I expected him to. If a new era of “assisted dying” were to dawn, he might not have had the option of assisted death because there was no specific time frame. And yet I believe this is exactly the kind of scenario where assisted death might make sense.
Because ultimately, the reason for allowing – and helping – someone to end their life should be based on the unbearableness of their condition, and not on an arbitrary assessment of life expectancy.
It requires a patient to have normal cognitive function and a judgment will have to be made by the professionals based on a submission from the patient about the intolerability of his predicament.
It seems bizarre to me that we are given an abundance of choices in almost everything, except our death. But if there is to be a change in the law, it is essential that we do not base it on a haphazard assessment of the time a patient has left.




