Experts say one in 10 dementia patients may be misdiagnosed, with the condition being a common one caused by poor diet and alcohol consumption.



Experts say more than one in 10 people diagnosed with dementia may have a common, treatable liver condition that causes similar symptoms.
That means thousands of people have been wrongly told they have the incurable memory-destroying disease, when in fact their problems are reversible, they add.
A study of more than 68,000 people with dementia found that nearly 13 percent showed signs of brain poisoning, also known as hepatic encephalopathy (HE).
This is caused by cirrhosis of the liver, where scar tissue builds up in the organ. This is usually the result of excessive drinking, obesity, or the viral infection hepatitis.
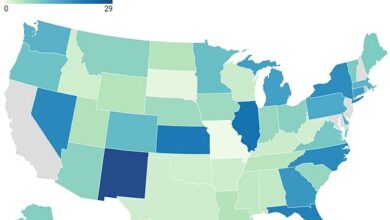
The new findings confirm research published in February that found about 10 percent of U.S. veterans with dementia may have HE.

Dr Rob Howard, professor of geriatric psychiatry at University College London, told MailOnline in an interview: ‘No one should be diagnosed with dementia without ruling out physical causes for the confusion.’

Early symptoms of hepatic encephalopathy include confusion, forgetfulness, changes in personality or mood, changes in sleep patterns, and difficulty writing – which are also symptoms of dementia.
However, British dementia experts have their doubts about this suggestion. According to them, there are indeed subtle differences between HE and dementia that doctors would notice.
Liver cirrhosis affects around 18 per cent of men and 11 per cent of women in the UK and causes fatigue, nausea, swollen limbs and itchy skin.
VS STATUS
Because scarring prevents the liver from properly filtering toxins from the blood, they build up and can damage the brain, leading to hepatic encephalopathy.
Early symptoms include confusion, forgetfulness, changes in personality or mood, changes in sleep patterns, and difficulty writing. These are also symptoms of dementia.
As the disease progresses, it can also cause unusual or slow movements, shaking hands and arms, extreme anxiety and severe confusion, slurred or slurred speech, and seizures.
Unlike dementia, which only gets worse over time, hepatic encephalopathy can be completely reversed with proper treatment.
This includes specific antibiotics and nutritional supplements.
Study author, Virginia-based gastroenterologist Dr. Jasmohan Bajaj, said: ‘We need to raise awareness that cirrhosis and related brain complications are common and silent, but treatable when detected.
‘Due to the aging of the population, the chance of overlap between hepatic encephalopathy and dementia has increased. This must be taken into account.’
He added: ‘Undiagnosed cirrhosis and possible hepatic encephalopathy may be a treatable cause of or contributor to cognitive impairment in patients diagnosed with dementia.’
Liver cirrhosis also increases the risk of liver cancer, which is another important reason to be aware of it, Dr. Baja says.
A recent report found that around one million people in the UK have some form of dementia, with this number expected to rise to 1.4 million by 2040.
According to estimates from the U.S. Centers for Disease Control, 5.8 million Americans currently suffer from Alzheimer’s disease and related dementias, the vast majority of whom are over the age of 65.
In the new study, Dr. Baja and colleagues analyzed data from 72 U.S. health care providers on 68,807 patients, mostly in their early 70s, who were diagnosed with dementia between 2009 and 2019.
No one had previously been diagnosed with cirrhosis. The team looked at the results of blood tests for levels of certain compounds to help them calculate a Fibrosis-4, or FIB-4, score — a common test for cirrhosis.
Commentary on the research for Medscape Medical NewsAccording to liver specialist Dr. Nancy Reau of Rush University Medical Center in Chicago, doctors may not realize that liver disease leads to cognitive decline.
“By using simple tools like FIB-4, you can make sure that you don’t overlook liver disease as a contributing factor in a patient with neurocognitive symptoms.”
Dr Rob Howard, professor of geriatric psychiatry at University College London, told MailOnline in an interview: ‘Full-blown hepatic encephalopathy looks different to dementia.
‘The symptoms of hepatic encephalopathy fluctuate in a way that they do not in Alzheimer’s. Anyone who works in a memory clinic will be familiar with this.
‘No one should be diagnosed with dementia until a physical cause for the confusion has been ruled out.
‘Simple tests should always be performed, including a liver function test.
“But I don’t think it’s credible to say that people with dementia have been misdiagnosed, based on this evidence.”