First UK case of ultra-deadly monkeypox strain hits London patient



A case of the new deadly strain of monkeypox that has struck several African countries has been discovered in London, the first in Britain.
The unnamed patient was on holiday in an African country currently experiencing an outbreak earlier this month.
They developed flu-like symptoms on October 21 and developed a rash three days later.
In search of medical advice, the case was flagged to the UK Health Security Agency (UKHSA) as possibly the new source of concern for mpox, called ‘clade 1b’.
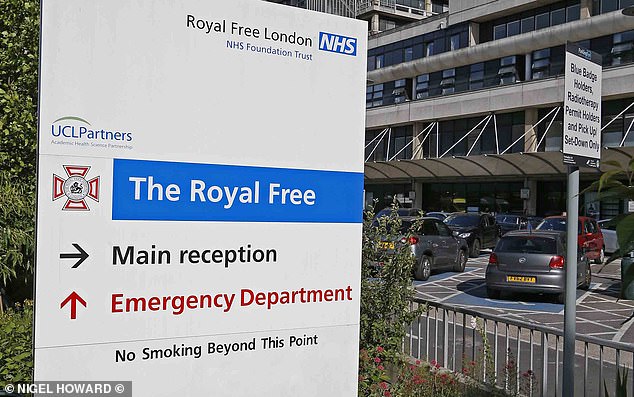
Laboratory tests confirmed that the patient did indeed have the disease and they are currently being treated by specialist staff at the Royal Free Hospital in London.
No further details are known about the patient’s condition.
UKHSA said they are currently tracing ‘less than 10’ people who are believed to have had close contact with the patient during the potential period he was infectious.
Officials do not currently suspect the patient was contagious during the flight back from the as-yet-unnamed African country where they contracted the disease.
How the patient acquired the new MPOX variant, which can kill around one in 20 adults infected with it, is currently unknown, although skin-to-skin contact is suspected.

The patient is currently being treated by specialist staff at the Royal Free Hospital in London
UKHSA said they are currently in discussions with their counterparts in the African country for contact tracing there and so are not revealing exactly which country is involved.
Officials say they still consider the threat clade 1b poses to the public to be “low.”
Professor Susan Hopkins, chief medical adviser at UKHSA, said: ‘Thanks to our surveillance we have been able to detect this virus.
‘The risk to the UK population remains low and we are working quickly to trace close contacts and reduce the risk of potential spread.
‘In accordance with established protocols, investigations are underway to determine how the individual acquired the infection and to assess whether there are any further related cases.’
Dr. Jake Dunning, infectious disease consultant at the Royal Free, added: ‘Our unit is run by a highly trained and experienced team of doctors, nurses, therapists and laboratory staff and has been specifically designed to ensure the safety of staff and other patients. .’
The rest of the NHS hospital is functioning normally.
Health and Social Care Secretary Wes Streeting added: ‘The overall risk to the UK population currently remains low and the Government is working with UKHSA and the NHS to protect the public and prevent transmission.’

A woman cares for her baby suffering from a severe form of MPOX in eastern Democratic Republic of Congo
Steve Russell, NHS national director for vaccination and screening, also said: ‘The NHS is fully prepared to respond to the first confirmed case of this clade of mpox.
Since the outbreak began, Clade 1b has spread through Central Africa, killing at least a thousand people.
Countries such as the Democratic Republic of Congo have been hit particularly hard, with cases also seen in Burundi, Rwanda, Uganda and Kenya.
The case of Britain now means that the country joins countries such as Sweden, Thailand, India and Germany in having business outside Africa.
Clade 1b is considered much deadlier than the clade 2 strain, which spread worldwide in 2022 and mainly affected gay and bisexual men.
The strain is estimated to cause death in about 5 percent of adults who contract the disease, but in children the mortality rate is as high as one in ten.
By comparison, Clade 2 only killed about one in 500 people who caught it.
However, experts say the death rate of clade 1b from Central Africa is unlikely to be repeated in developed countries such as Britain, due to greater access to higher quality healthcare.

The smallpox vaccine is known to help prevent MPox because the two viruses are closely related
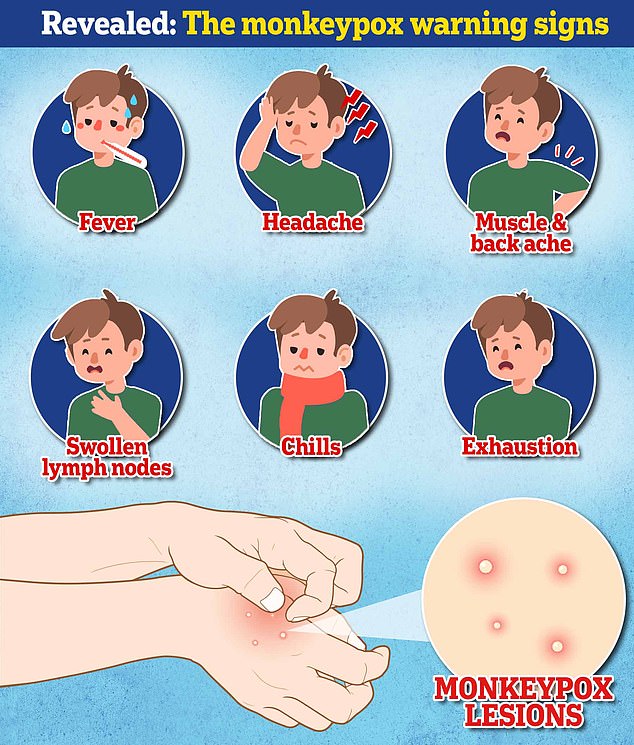
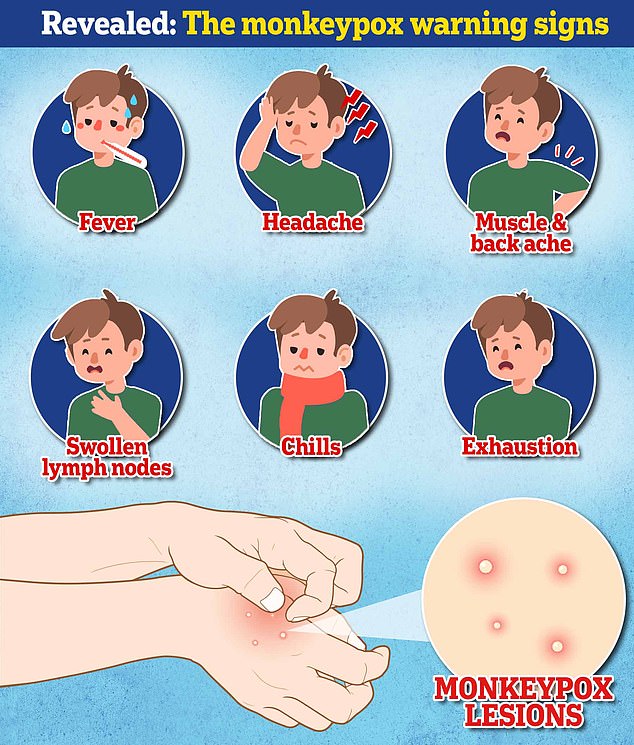
Common symptoms of MPOX include a rash or pus-filled lesions that can last for two to four weeks.
In a small number of cases, the infection can invade the blood and lungs, as well as other parts of the body such as the brain, making it life-threatening.
The infection is mainly transmitted through close personal contact with someone who is infected or through contact with contaminated materials such as bedding.
Anyone with symptoms should continue to avoid contact with other people while symptoms persist.
It can also cause fever, headache, muscle aches, back pain, low energy, and swollen lymph nodes.
UKHSA also said they are securing more supplies of MPox vaccines as part of the jab’s further rollout.
Current MPOX vaccines, which are designed to work against smallpox, a close relative of the MPOX virus, were used against the milder variant during the 2022 outbreak.
But they have yet to be widely tested against the more potent clade 1b strain.
Diseases such as clade 1b mpox are treated in so-called ‘high consequence infectious diseases’ units in the NHS, such as those at The Royal Free.
The Royal Free treated Ebola patients in this department in 2015.