How a new hi-tech pacemaker with a 25-year battery life saved Emily Coles’ life – after she fainted out of nowhere



After Emily Coles suddenly collapsed at home, she had to put her life on hold while doctors investigated the cause.
Emily now knows her heart stopped beating for ten seconds, but at the time she had no idea her life was in danger.
Emily, 24, had been having coffee with her older sister Lauren in her kitchen last September when she fell to the floor.
“One minute we were having a conversation, the next I was on the floor,” says Emily, a nurse, who lives with her mother Karen, 56, and father Nigel, 58, in Rotherham, South Yorkshire.
“All I remember was feeling a little light-headed.” Lauren, 28, who is training to be a doctor, was so concerned she took Emily to A&E where she was seen by a specialist cardiac physiologist.
Emily underwent tests, including an electrocardiogram and a tilt test, in which the patient lies flat on their back on a motorized table, which tilts to a near-vertical position for 45 minutes.

After Emily Coles (pictured) suddenly collapsed at home, she had to put her life on hold while doctors investigated the cause
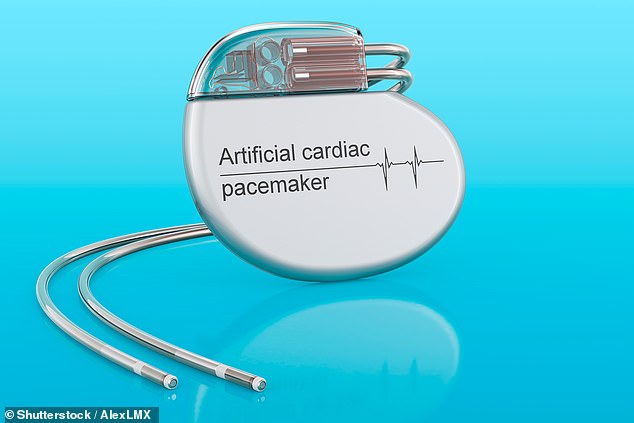
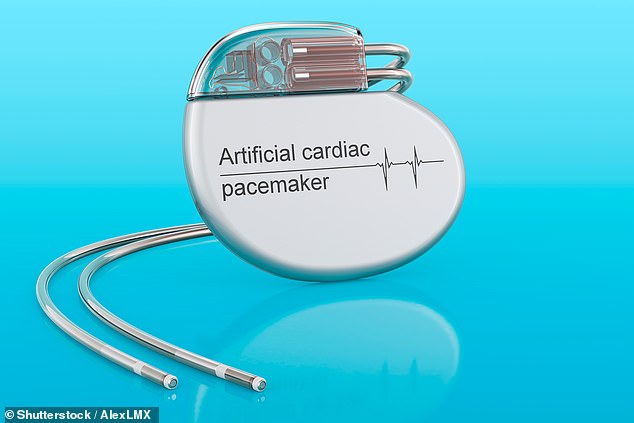
She was diagnosed with reflex syncope, in which the heart slows down so much that it leads to temporary loss of consciousness (syncope is the medical term for fainting). Emily was one of the first to receive a new hi-tech pacemaker, which comes with a 25-year battery life
Heart rate and blood pressure are continuously monitored to see how different positions affect the patient’s heart.
After sitting upright on the tilting table for half an hour, Emily suddenly fainted. As she did so, the monitors showed her heart had stopped beating.
She was diagnosed with reflex syncope, in which the heart slows down so much that it leads to temporary loss of consciousness (syncope is the medical term for fainting).
Worryingly, Emily’s heart stopped for ten seconds or more at a time.
She was told she needed a pacemaker, becoming one of more than 500,000 people in Britain who get a pacemaker every year.
But Emily was one of the first to receive a new high-tech pacemaker, which comes with a battery that should last 25 years – more than twice as long as previous models – and has a lower risk of complications.
Although doctors don’t know what caused Emily’s condition, she now remembers feeling dizzy at times in the two years before. “I had to hold on to something to keep myself stable,” she says. But at the time, tests, including an echocardiogram (an ultrasound scan to inspect the heart), had turned up nothing.
After her breakdown and diagnosis last year, Emily was banned from driving.
This made it harder for her to go to work – and her 12-hour shifts in a busy hospital – and it also deprived her of her social life and made her nervous about going out.
She was also told to drink more water and eat more salt, both of which help maintain blood pressure and avoid the dips that can lead to fainting.

The implant has a battery and electronic chips all housed in the compartment. Crucially, the battery has a much longer lifespan than conventional pacemakers – up to 25 years.
But to manage her condition in the long term, heart specialists at Sheffield Teaching Hospitals NHS Foundation Trust, where Emily (pictured) was treated, said she should be fitted with a pacemaker to prevent future life-threatening collapses.
A pacemaker is usually implanted through a small 5 cm incision on the left side of the chest. The wires connecting the pacemaker to the heart are fed to the heart via a vein, before the pacemaker is placed just below the collarbone.
The device detects through the wires what the heart is doing, and if it slows down or misses a beat, the pacemaker delivers an electrical impulse to return the heart to its normal speed.
The disadvantages of conventional pacemakers include that the leads may not function properly. They also only last about ten years before they need to be replaced.
For Emily, this could mean multiple replacements throughout her life, leaving her vulnerable to the risks of surgery, such as infection and sepsis.
A 2019 study from Manchester University NHS Foundation Trust, published in the journal PLOS One, found that the Trust treated 84 cases of pacemaker-related infections over a two-year period, with half of these patients requiring emergency surgery.
Not only were patients’ lives at risk, but it also cost the charity almost £25,000 per patient to tackle the problem.
Dr. Nigel Lewis, a cardiologist who treated Emily, said: ‘We are trying to prevent young people from getting pacemakers because they need to be replaced.’
However, Emily’s pacemaker, which is about the size of an AAA battery, requires less invasive surgery and carries fewer risks.
The implant has a battery and electronic chips all housed in the compartment. Crucially, the battery has a much longer lifespan than conventional pacemakers – up to 25 years.
There are also no cables, avoiding the type of failure that requires the pacemaker to be replaced.
A pacemaker is usually implanted through a small 5 cm incision on the left side of the chest. The device detects through the wires what the heart is doing, and if it slows down or skips a beat, the pacemaker delivers an electrical impulse to return the heart to its normal rhythm
In January, Emily became one of the first patients in Britain to have the leadless pacemaker fitted in an hour-long procedure under local anaesthetic.
A thin tube (a catheter) was inserted into a vein in her leg and guided to the right ventricle – one of the two lower chambers of the heart.
The doctors then passed the small pacemaker through the tube and attached it with small hooks to the septum, the tissue wall that separates the right and left chambers.
In a two-year trial, the leadless pacemaker, developed in the US, was found to be as effective as traditional devices.
Dr. Lewis says: ‘It could be a game-changer for younger patients and for people on kidney dialysis who have long-term lines in their bodies.
‘If it becomes infected, a traditional pacemaker can easily infect these lines as well.
‘In some breast and lung cancer patients who receive radiotherapy, the treatment can cause blockages in the arteries, making it difficult to fit a traditional pacemaker.
“So this new pacemaker could benefit hundreds of patients initially, but in the long term it will benefit thousands.”
For Emily it has been life-changing. “I found it difficult to accept that I needed a pacemaker at the age of 24,” she says.
‘Sometimes I feel it moving in time with my heart, which feels like a strange vibration at the base of my neck.
‘But I feel like I have my life back on track. I’m riding again and have reinstated my gym membership. Before my diagnosis, I took it all for granted, but I’m so excited to be active again.”




