How a wave of new forms of dementia could be fueled by a surprising culprit, every home is facing it



A new study has fueled concerns that America could see a surge in dementia in the coming years and decades due to COVID.
It found that nearly two-thirds of people over 65 who were hospitalized with the virus developed mild cognitive impairment, which can be a precursor to dementia.
Independent experts told DailyMail.com that this is a trend they are closely watching, because if there is a link, it could affect millions of elderly people infected with the virus in the near future. But the new study does not go beyond concluding that the two are linked, experts warn.
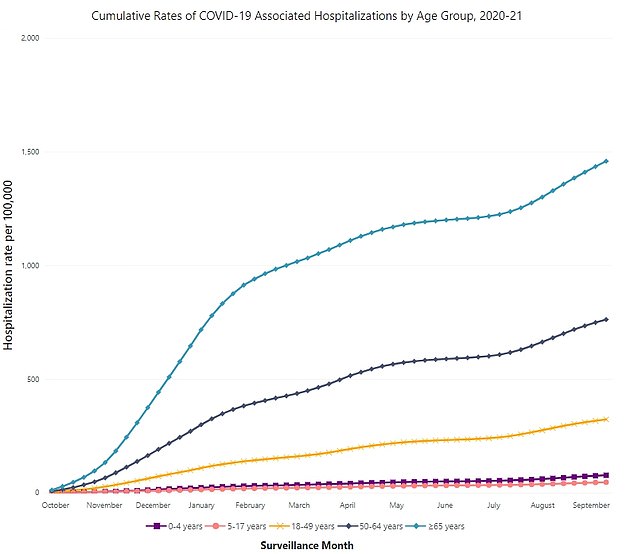
CDC data shows this age group accounted for 47 percent of all hospitalizations in 2020-2021, or approximately 1,701,300 people.

The study looked at people over 65 who were hospitalized with COVID-19 in 2020. This means their study population was very sick, and it’s hard to say how people with less severe illness might be affected.
Data from the CDC’s COVID-Net lab showed the cumulative number of COVID hospitalizations from 2021 to 2022. Studies have estimated that about 1,701,300 people over the age of 65 have been hospitalized this year.
The researchers from the University of New South Wales came to these conclusions in their study by reviewing 18 older studies. This represented approximately 412,900 participants who had been hospitalized with COVID-19 and 411,900 healthy participants – both groups were all over the age of 65.
The research was published as a pre-evidence, meaning it has yet to be reviewed by other scientists, in the journal Aging Research Reviews.
About 65 percent of people with the virus had some degree of mild cognitive impairment, a type of brain fog that can sometimes be a precursor to dementia.
Researchers aren’t sure why COVID causes these changes in the brain, but they suspect it could be related to inflammation or changes in blood flow, Dr. Vin Gupta, a pulmonologist and public health physician who was not involved in the study, told DailyMail.com.
However, Dr. Gupta and other independent experts have also raised concerns about the study. The studNo other factors that increase the risk of dementia, such as high blood pressure, heart disease and obesity, were ruled out.
“This is another study that provides direction and some additional insight into what may be happening with COVID and its impact on human organ function, but I think it’s far from definitive,” he said.
Doctor Eve Elizabeth PennieGP and Drugwatch medical officer who was not involved in the study told DailyMail.com she had found similar weaknesses in the research.
However, it is further evidence of a trend that public health experts have been observing for some time.
“Given the mounting evidence from similar studies, the findings are compelling and somewhat expected,” Dr. Pennie said.
There are no previous studies that have concluded that COVID-19 causes dementia, but several previous studies have shown there may be a link between the two, Dr. Gupta said.
Many diseases have secondary effects, such as the link between chickenpox and shingles, so it is reasonable to suspect that this virus may also have consequences, experts say.
In previous outbreaks of similar viruses, such as SARS in 2003 and MERS in 2012, researchers noted that cognitive impairment was a side effect.
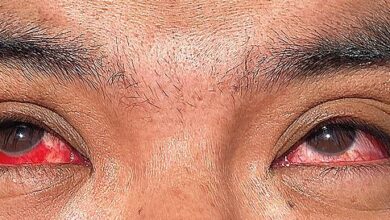
COVID-19 causes a host of changes in the body, including increased inflammation and changes in blood pressure and blood clotting, both of which can trigger changes in the brain, the study authors wrote.
In addition, COVID-19 can also cause more serious neurological disorders in rare cases. conditions such as encephalitisa swelling of brain tissue that kills or damages parts of neurons.
It’s less clear how COVID-19 might directly relate to dementia. The study authors suggest that the virus may increase the body’s levels of beta-amyloid, a protein that builds up in the brains of Alzheimer’s patients.

Dementia has been linked to COVID in a number of studies. But finding a link is not the same as proving a cause, Dr. Gupta warned
Otherwise, the changes in blood flow could cause frequent, small injuries to brain tissue, depriving it of oxygen often enough to cause long-term effects that could lead to dementia. Researchers aren’t yet sure what theory could explain this link, Dr. Gupta said.
Dr. Pennie noted that while these findings are in line with current trends, there are some major caveats.
First, the study did not take into account pre-existing conditions such as high blood pressure, diabetes and heart disease, all of which are common in people over 65 and increase the risk of dementia.
Second, most of the included studies did not have data from before their patients got COVID-19. This means that their cognitive impairment may have existed before they got the virus, and it is difficult to know what COVID actually did to them.
Moreover, most of the data were collected in 2020, before large-scale vaccination, and all patients studied had a very severe case of the disease, having been hospitalized with it.
This makes it impossible to apply what we’ve learned here to today’s general population, who are more likely to be vaccinated and have a less severe case of COVID-19, Dr. Gupta said.
Overall, while the study points to some trends, Dr. Gupta said, “from a design standpoint, it is a very weak study.”