If the doctor says your illness is just stress

Amina AlTai had always prided herself on her drive and resilience. When she began to experience brain fog and fatigue, Ms. AlTai, 39, simply thought it was the long hours she was working in her marketing job. So she started writing down memories to keep herself on track. But then her hair started falling out, she gained and lost significant weight, and developed gastrointestinal problems.
Mrs. AlTai was sure something was wrong. But the first six doctors she saw didn’t take her seriously, she said. Some told her that she had so much hair that a little hair loss shouldn’t be a problem. Several people said she looked healthy and dismissed her symptoms as simply stress. It wasn’t until another doctor ordered blood tests that Ms. AlTai was diagnosed with Hashimoto’s disease and celiac disease, two autoimmune diseases that can damage the thyroid and small intestine.
“They called me and said, ‘Don’t go to work. Go to the hospital instead because you are just a few days away from multi-organ failure,'” Ms. AlTai recalled. The two chronic illnesses had disrupted her ability to regulate hormones and absorb essential vitamins and nutrients.
Scientists now know that stress is closely linked to many chronic diseases: it can cause immune changes and inflammation in the body that can worsen symptoms of conditions such as asthma, heart disease, arthritis, lupus and inflammatory bowel disease. Meanwhile, many problems caused by stress – headaches, heartburn, blood pressure problems, mood swings – can also be symptoms of chronic diseases.
For doctors and patients, this overlap can be confusing: Is stress the sole cause of someone’s symptoms, or is something more serious going on?
“It’s really hard to untangle,” says Scott Russo, director of the Brain-Body Research Center at the Icahn School of Medicine at Mount Sinai.
How Stress Can Cause Chronic Disease
Stress naturally triggers the so-called fight-or-flight response. When we encounter a threat, our… blood pressure and the heart rate increases, muscles tense and our bodies concentrate blood sugar levels to make it easier to respond quickly, said Dr. Charles Hattemer, a cardiovascular health specialist at the University of Cincinnati.
When people are stressed for weeks or months, their body can no longer keep up with other functions, leading to problems such as forgetfulness, fatigue and sleep problems. Stress hormones such as adrenaline and cortisol can increase blood pressure chronically or increase plaque depositswhich over time can damage the heart, Dr. Hattemer said.
There is also evidence that stress can contribute to over-activation of the immune system and lead to inflammation. In a study of 186 patients, researchers in Italy found that 67 percent of adults suffered from this celiac disease had experienced a stressful life event before their diagnosis.
More recently, Dr. Russo and his colleagues in two studies demonstrated that stressed mice higher levels of neutrophilsthat cause inflammation, and fewer T cells and B cells in the bloodstream that can produce antibodies or kill cells infected with viruses.
He and his colleagues also found patients with major depressive disorder had similar immune cell imbalances compared to healthy controls. Researchers believe the body changes the composition of immune cells circulating in the blood to reduce damage from infection or acute stress, Dr. Russo said.
However, when the body is faced with chronic stress, sometimes it “just can’t turn off the immune system,” Dr. Russo says.
For people who may already be at risk for chronic disease, whether due to their genetic predisposition, exposure to chemicals, air pollution, or viral infections, a prolonged period of stress can tip them over the edge into becoming ill.
Lynne Degitz, 56, has battled what seemed like extreme infections for years. Once, she thought she had mono. Another time, she was certain it was bronchitis. Neither she nor her doctors thought it could be a chronic illness.
Then she started a new, stressful job and suffered from fever, joint swelling and fatigue almost every day. “I had interesting and demanding work, so I just kept going,” Ms. Degitz said. “I would just use a short-term disability to recover or use vacation time to recover when I needed it.”
After more than two years of going back and forth to medical appointments and trying treatments that ultimately didn’t help, Ms. Degitz was diagnosed with a form of arthritis known as Still’s disease. Doctors aren’t sure what causes it, but… research seems to indicate that it is likely a combination of factors, including abnormal responses to infections and stress.
“We all have physical ailments and weaknesses,” Dr. Russo said. “Stress just exploits them and makes them worse.”
When symptoms become a source of stress
For patients with chronic illness, the same stressors that may have caused their symptoms can make it difficult to manage their condition.
And some said they don’t always feel like doctors realize how difficult it can be to manage stress, especially when they’re feeling sick. When Teresa Rhodes was first diagnosed with rheumatoid arthritis several decades ago, a doctor suggested she increase exercise to reduce her stress and strengthen her joints, which had been damaged by the disease.
But “the symptoms of the disease itself were stressors,” said Ms. Rhodes, who is now 66. “It’s very difficult to exercise when you’re so tired.” Only after other life stressors disappeared — her children were grown and she left a difficult marriage — was she able to get enough rest and eventually start exercising again.
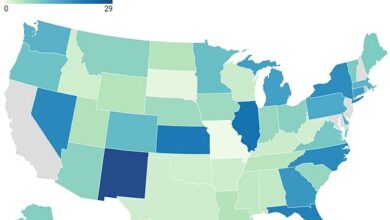
Many doctors aren’t trained to ask about sources of stress, or to counsel patients about the impact of stress, said Alyse Bedell, a clinical researcher who specializes in how stress affects digestion at UChicago Medicine. A 2015 study of more than 30,000 patient visits to doctors’ offices found that primary care physicians only counseled patients about stress management during 3 percent of visits.
When Stephanie Torres’ 12-year-old son Nico was diagnosed with Crohn’s disease, she was surprised to hear that the gastroenterologist thought managing the stress that clearly triggered his symptoms was the family’s responsibility. “Her response to me was basically, ‘This is your problem. Solve it.'”
Patients said that instead of simply suggesting that they eliminate sources of stress, doctors could work with them on small ways to manage stress every day. Once Ms. AlTai was diagnosed and began taking medications for both of her conditions, she felt well enough to make the dietary changes needed to address the nutrient deficiencies caused by her illnesses. She began taking regular morning walks and meditating.
Ms. AlTai eventually left her marketing job and became an executive coach, which allowed her to set her own schedule, she said. Her hospitalization and diagnosis with two chronic illnesses made her realize the changes were necessary.
“I call it my stopping moment because it literally stopped me in my tracks,” she said. “I really had to reevaluate my relationship with work, success and stress.”