If you think you have mpox, here’s what you should do



The World Health Organization has declared a global health emergency due to the MPOX epidemic (formerly known as monkeypox) in African countries such as the Democratic Republic of Congo, where the outbreak is concentrated. This is the second time in the past three years that the WHO has declared the MPOX epidemic a global health emergency.
“The current increase in mpox in parts of Africa, together with the spread of a new sexually transmitted strain of monkeypox virus, is an emergency not only for Africa but for the whole world,” said the chair of the WHO committee, Professor Dimie Ogoina, in a press release“Mpox, which originated in Africa, was neglected there and later caused a global outbreak in 2022. It is time to take decisive action to prevent history from repeating itself.”
Below you will find guidelines on what to do if you are sick with mpox or have come into contact with it.
What to do if you have been exposed to mpox
Anyone who has been in contact with a person (or, less likely in the current outbreak, an animal) should monitor themselves for symptoms for 21 days, according to the U.S. Centers for Disease Control and Prevention. You do not need to isolate (stay away from others) unless you develop symptoms.
Exposure likely means you’ve had direct skin-to-skin contact with someone who has mpox, as that’s the main way it spreads. However, you can also get mpox by touching clothing or other things that the person’s rash may have come into contact with, or through respiratory secretions. Some scenarios in which mpox can be transmitted include sex, kissing, coming into contact with someone’s rash or sores through a hug, or sharing a towel, bed, or clothing. Mpox can also spread through prolonged face-to-face contact; researchers are studying whether it spreads in bodily fluids such as semen and vaginal fluid.
Get vaccinated if you can
If you have been exposed to mpox in the past two weeks and have no symptoms, you should contact your local health department to see if you can get a vaccine. Jynneos vaccineThe vaccine is most effective if given within four days of exposure, but may be effective in reducing the severity of symptoms if given between four days and two weeks after first exposure.
While the criteria for who can get a vaccine varies by city depending on the level of spread in a particular area, if you have been exposed, chances are good that you live in an area where the vaccine is offered.
If you are at higher risk for serious illness from mpox (for example, if you have an immunocompromised condition), contact your doctor to see if there are additional treatments available to you or if there are any other steps you should take after exposure.
Watch for symptoms
At this time, the CDC says you can continue your daily activities if you have been exposed to mpox, but have no symptomswhile you continue to monitor and keep an eye on them. The monitoring period is 21 days or three weeks. You do not need to isolate because you are not infectious until symptoms start (if they do). Common symptoms of mpox include fever, swollen lymph nodes, or a new skin rashYou may also have pain in your anus or mouth if the rash spreads there.
The CDC also recommends taking your temperature twice a day to check for a fever.
But if you develop symptoms, your next steps will depend on the type of symptoms.
If you notice symptoms and start to feel sick (but do not have a rash or new rash) lesion): Let’s say you develop a fever, swollen lymph nodes, or another symptom but no rash. You should isolate (stay home and try to avoid other people) for five days, according to the CDC, even if that puts you over the 21-day monitoring limit. If you haven’t developed any other symptoms or a rash after five days, you can end your isolation, according to the CDC.
If you notice symptoms and develop a rash: Avoid close contact with people, isolate yourself at home if possible, and follow the guidelines in the next section.

While you are recovering from mpox, you should avoid shaving near the rash to avoid spreading the virus to other parts of your body.
What to do if you have mpox
If you have been to the doctor and a test has confirmed that you have mpox, or if you have been directly exposed and have all the symptoms of mpox, you should: isolating from other people and stay home (if you can) until your symptoms go away, according to the CDC. That also means avoiding public transportation, where you may be in close contact with other people’s bodies.
But mpox can be a long-term illness (about two to four weeks) and if you can’t be completely isolated for that long, most important things you need to do According to the CDC, these include: making sure to completely cover the rash or lesions with bandages and clothing, wearing a well-fitting mask if you must be around other people, avoiding close contact with others, avoiding crowded spaces, washing your hands often, and staying isolated if you have other symptoms, such as fever or respiratory symptoms.
you are considered contagious until your sores or rash crusts over and a new layer of skin forms. You should also call your health care provider right away to determine next steps, including whether you need to come in for additional treatment.
How do I know if I have mpox?
Symptoms usually appear within three weeks of close contact with a person who has mpox. Common symptoms of mpox include:
- A rash or spots on the body, including the genital area, anus, hands, face, chest, or mouth. For some people, the sores can be very painful.
- Fever
- Swollen lymph nodes
- shivers
- Exhaustion
- Muscle pain
- Respiratory symptoms such as coughing or a stuffy nose
You may experience all or just some of these symptoms. People who experience flu-like symptoms usually develop a rash one to four days after they start feeling sick.
The only way to confirm a case of mpox is to get tested by a health care provider, who swabs the lesions. Testing capacity is improving in the U.S., but it may still take some time to get your results. While you waitAccording to the CDC, you should remain in isolation as long as you have symptoms.

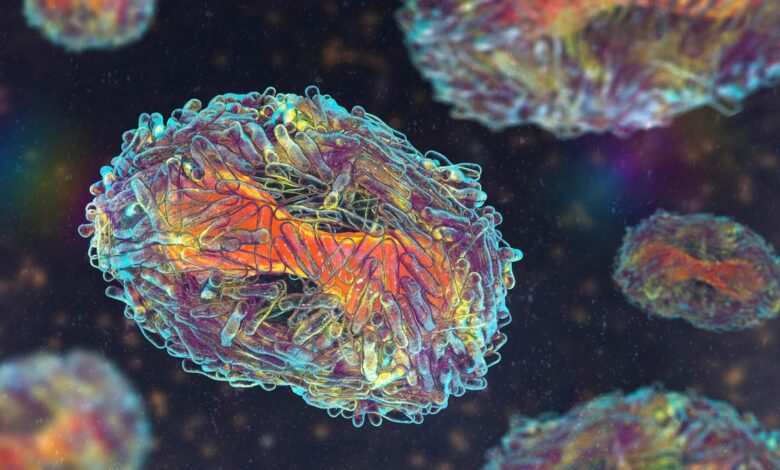
Some examples of monkeypox lesions.
Isolate at home
The CDC guidelines for home isolation For people with mpox, this includes avoiding close contact and intimacy with people (hugging, kissing, sex, etc.). The agency also says to avoid sharing linens and towels. (Like the towel in the bathroom that you dry your hands with.)
If you live with other people and are around them at home, you should wear a mask for extra protection. (This mask contains your respiratory droplets.)
If you have no choice but to go outside or if you live with other people, make sure to cover the rash or sores with well-fitting clothing, such as pants or a long shirt. If the rash has spread to your hands, wear gloves.
If possible, it is wise to use a different toilet than other family members. Also avoid sharing food, dishes and cutlery.
If using the same toilet is the only option, the person with mpox should disinfect shared areas (toilet seat, shower, bathroom vanity, etc.) with disinfectant after use and wear gloves when necessary, the CDC says.
Personal Care Tips
If you wear contact lenses, you should not wear them when you are sick to avoid accidentally infecting your eyes with mpox, the CDC says. If you shave, you should avoid shaving any parts of your body that are covered in the rash for the time being.
Pox viruses such as mpox can survive on clothing and surfacesaccording to the CDC, which is why it’s important to disinfect things you’ve touched while you’re contagious. While it’s not entirely clear how big the risk is of spreading it in public places, there are precautions you should take if you do your laundry in a public laundromat. New York City has its own manual for doing the laundry yourself with mpox, and the CDC advises contacting your local health department to find the best “laundering option.”
Avoid contact with animals
Unfortunately, mpox is a zoonotic disease, meaning it is transmitted from animals to humans. That means there is a chance that you can infect your dog, cat or other pet that is a mammallike a rat. (Non-mammals such as reptiles, birds, and fish are unlikely to get mpox, according to the CDC.)
If possible, the CDC advises, have someone else care for your pet while you are sick or recovering from mpox. If that is not possible, keep pets away from your bandages, bedding, towels or other materials that could be contaminated.
If you notice your pet acting differently or think it has become ill after contact with someone with mpox, contact your veterinarian or animal health official.

If possible, have someone else watch your pet while you recover from monkeypox, the CDC says. If that’s not possible, try not to touch your pet, keep your rash covered and your mask on, and also keep your pet away from clothing or linens that may have come into contact with your rash.
Do I need treatment for mpox?
Most people with mpox do not need additional treatment and are advised to stay home and manage symptoms. However, some people have lesions that are quite painful, in which case you should call your doctor for help with pain management, Dr. Bernard Camins, the medical director of infection prevention at Mount Sinai Health System, told The New York Times that a doctor can recommend sitz baths or stool softeners if necessary.
While most people will recover at home, there are also people who… be at higher risk of serious illness or may need additional treatmentincluding people with weakened immune systems, children under 8, pregnant or breastfeeding women, and people with skin conditions such as eczema or psoriasis, the CDC said.
There are a few medications or antivirals which the CDC lists as possible treatments for mpox in some patients. For example, tecovirimat (TPOXX) and brincidofovir are both approved for treating smallpox and are also reported to work against mpox.
If you think you are at higher risk for a serious illness and your doctor has not yet offered you treatment options, ask what your options are.




