It’s not just women hit by medical sexism… men too are being ignored because they have ‘female’ illnesses, argues Dr Philippa Kaye. So what are these illnesses and what can be done?



I have spent much of my career as a GP championing women’s health. It’s something I feel passionate about – because women are so often poorly served by the NHS and medicine in general.
We are half of the population – yet just 2 per cent of research is focused on female reproductive health, pregnancy and childbirth.
And, until recently, subjects such as incontinence, sexual dysfunction in women and the menopause – something that every women will go through – were little talked-about.
Thanks to campaigners and, more recently, celebrities opening up about their own issues, these subjects are less taboo. But there is a group being left behind that I think we need to talk about: men.
In a week where research has shown that women are unnecessarily dying of heart disease, due to misconceptions it’s a man’s problem, this might seem an odd thing to write. But hear me out: some men are just as affected by this kind of medical sexism.

Women are so often poorly served by the NHS and medicine in general. We are half of the population yet just 2 per cent of research is focused on female reproductive health, pregnancy and childbirth
Specifically, men who suffer from what are normally through of as ‘women’s problems’.
Over the years I’ve become aware that this group are, just like women, being dismissed, fobbed off, misdiagnosed and generally given the run-around in trying to get a diagnosis and treatment.
My colleague Dr Ellie Cannon wrote about the issue in her column last week – and we have been inundated with responses from readers who’ve been affected.
Take Jim Fraser, 78, who developed bone-thinning disease osteoporosis – which primarily affects women – due to cancer treatment.
Despite having suffered a number of fractures in his spine he’s been barred from having a new osteoporosis drug called abaloparatide because it’s not been NHS approved for male patients.
‘It’s incredibly frustrating, and worrying knowing my spine is constantly at risk,’ he told us.
So what are the ‘women’s illnesses’ that also affect men, how can they be spotted and what can be done about them?
Men blighted by the burn of cystitis
Urinary tract infections – UTIs – are uncomfortable and sometimes painful conditions which develop when bacteria get into the parts of us involved in making urine and carrying it out of the body.
Symptoms include a frequent urge to urinate and a burning sensation when going to the toilet.
If infections become chronic, they may cause inflammation and scarring of the bladder.
More than half of women will develop a UTI in their lifetime – but men are also affected.
So men get it too?
One in ten men will suffer a UTI, although it’s less common because of male anatomy.
Women’s urethras – the tube where urine flows out from the bladder – are shorter than men’s and closer to the anus, which makes it easier for bacteria to enter and make their way into the bladder.
However studies show men with UTIs are more likely to end up with serious complications such as kidney infections, inflammation of the prostate known as prostatitis, and sepsis.
Men, like women, are more likely to develop a UTI after 50.

Former Deputy Prime Minister John Prescott has spoken openly about his battles with eating disorders
While in women it’s linked to a reduction in levels of the sex hormone oestrogen, which affects the tissues of the genitals and urinary tract, in men the risk is linked to an enlarged prostate, also known as benign prostatic hyperplasia (BPH). This affects 50 per cent of men over 50 and causes the prostate to press on the urethra, meaning that the bladder may not empty fully, allowing bacteria to build up.
It can also be linked to diabetes and kidney stones. Interstitial cystitis, which can cause more intense and chronic symptoms, including needing to urinate up to 60 times a day, is also up to five times more common in women. But studies suggest it’s also under-diagnosed in men because fewer seek help.
How men can get help
Speak to your GP who will want to take a urine sample and may want to rule out other conditions such as prostatitis, or bladder or kidney cancer.
Once diagnosed, men need a longer, seven-day course of antibiotics – compared to just three days for women – because they’re more at risk of further complications.
If you’re over 50, it’s a good idea take steps to reduce your risk
of an enlarged prostate by exercising regularly and limiting alcohol and caffeine to prevent UTIs in the first place, as these can irritate the bladder and worsen urinary symptoms.
Intimate problem often misdiagnosed
Lichen sclerosus is a chronic inflammatory skin condition which can causes itchy white patches, pain and swelling in the genitals.
It isn’t contagious or sexually transmitted, but it can cause huge discomfort when urinating or having sex – and around one in 20 women with the condition will develop vulval cancer.
But experts increasingly think penile cancer may be due to undiagnosed lichen sclerosus.
So men get it too?
Absolutely, although it’s much less common. Around one in 1,000 men suffer from it, compared to one in 80 women. And while for women it tends to hit between 40 and 60, it can affect boys or men of any age.
It’s most often seen on the foreskin and tip of the penis where the skin may feel uncomfortable, itchy, burning and sore, especially during or after sex.
The foreskin can get tighter, leading to painful erections, and skin may tear and bleed during sex. The skin can look red with cracks, sores or small blisters, and over time, it may turn white.
But many men are probably being misdiagnosed with infections or suffering in silence with something which they – and even their doctors – don’t understand because of a lack of awareness.
The cause of lichen sclerosus isn’t fully understood. In women, it may be an auto-immune condition – where the body mistakenly attacks healthy cells. But in men, it’s thought tiny amounts of urine trapped under the foreskin after urinating may be a trigger – men who were circumcised early in life almost never develop it.
How to get help
Don’t ignore it or just buy an anti-fungal or steroid cream for the itching – they won’t work – and it won’t go away on its own.
Around 8 per cent of cases
may also develop into penile cancer, another reason to get prompt treatment.
See your GP, who might want to carry out tests to rule out an infection, including STIs.
If this comes back negative and treatments like antifungals don’t quickly resolve the issues, a referral to a dermatologist or urologist is needed.
Treatment is the same as for women and involves using powerful steroid ointments. But if this does not work, circumcision may also be recommended, which tends to be curative.
Bone thinning that can be a killer
Osteoporosis is a disease which causes the bones to become more porous and fragile, which increases the risk of fractures.
It develops slowly over several years and is often known as the ‘silent’ disease, because it is often only diagnosed after a fall which causes a bone, most commonly a hip, wrist or a vertebrae in the spine, to break.
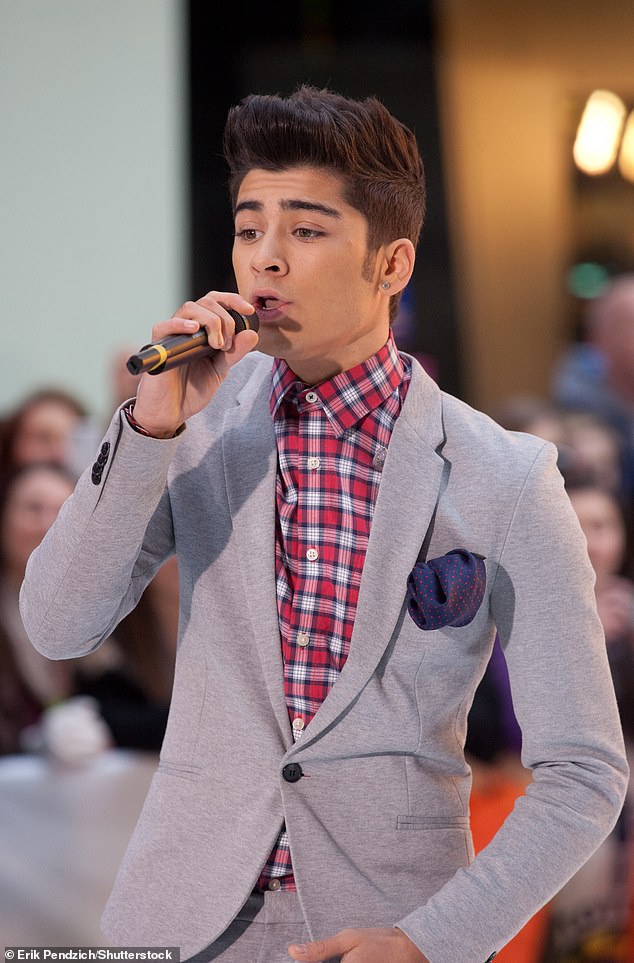
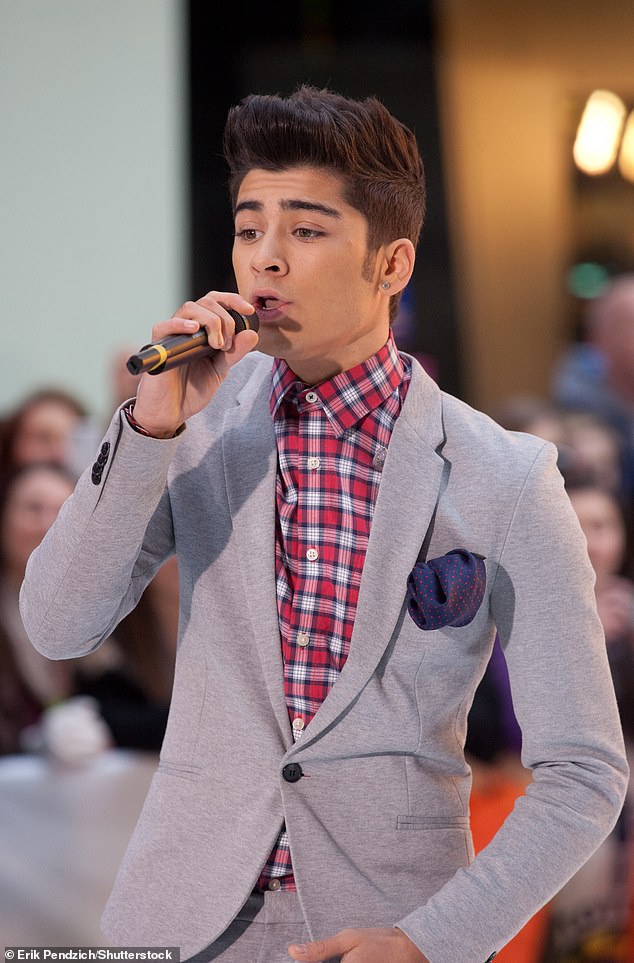
One Direction star Zayn Malik has also spoken openly about his problems with eating disorders
It’s more common in women because levels of the sex hormone oestrogen – which prevents bones from getting weaker – fall after menopause, and women lose on average 10 per cent of their bone mass in the first five years.
But other risk factors include cancer treatment, having an overactive thyroid gland, smoking and excessive alcohol use.
So men get it too?
Yes – studies suggest one in five men are affected as they get older, compared with around half of women over 50. It develops later in life in men – generally not until 70 or over – because they start off with greater bone mass.
But because it is often seen as a women’s disease, men who suffer a fracture are less likely to be evaluated for osteoporosis.
And statistics show that, while fractures may be more common in women, they can be more serious in men, partly because they may coincide with more frailty overall – 37.5 per cent of men died in the year after a hip fracture, compared with 28.2 per cent of women, one study found.
While men continue producing the male sex hormone testosterone into old age, those who are deficient are thought to be more at risk because low levels are linked with a reduction in bone density.
How to get help
Unfortunately for many, osteoporosis is only diagnosed after a fracture – and even then, there is a postcode lottery for screening. The Mail on Sunday is running a campaign to expand access to crucial fracture liaison services which would offer screening for the disease to anyone over 50 who breaks a bone.
If you do suffer a fracture in middle age or older – man or woman – ask to be screened for osteoporosis.
Even when a diagnosis is made in men, not every treatment option is available to them.
As I mentioned in my introduction, abaloparatide, which stimulates the cells to increase bone density, isn’t offered to men due to limited evidence. Treatments which are available include bisphosphonates, which slow the rate at which bone breaks down.
Body image illness that hits both sexes
Eating disorders are complex mental health conditions which involve eating too much or too little, often to cope with difficult feelings or situations. They affect 1.25 million people in the UK.
The most common are anorexia, which typically involves eating too little or exercising too much, and bulimia, which involves over-eating and then taking drastic action to avoid putting on weight, such as vomiting, taking laxatives or over-exercising.
We typically associate these problems with girls and women but this means men living with them often fall through the cracks.
So men can suffer too?
Yes – but stereotypes means fewer men seek help, and much less research has been carried out on men, according to eating disorder charity Beat. Research suggests around 2 per cent of men are at risk of developing an eating disorder in their lifetime, compared with 8 per cent of women.
But this is likely to be a huge under-estimate. Beat suggests it’s more realistic to suggest one in four with an eating disorder is male. Men are also more likely to develop a binge eating disorder than women. And there is some evidence from US organisations to suggest diagnoses in men are increasing at a faster rate than in women. But this may be because awareness is beginning to change.
Several high-profile men including former England cricketer Freddie Flintoff, One Direction star Zayn Malik and former Deputy Prime Minister John Prescott have spoken openly about their battles with eating disorders.
How to get help
It’s very difficult for people with eating disorders to get better on their own. And the sooner someone is treated, the better their chance of a full recovery.
In England you can get advice from Beat by calling their helpline on 0808 801 0677 or emailing help@beateatingdisorders.org.uk.
And get in touch with your GP, who can refer you for further assessment by a specialist eating disorder service. Treatment is likely to include talking therapies and support groups, but there could be a wait to be seen.
Cancer that hit Beyonce’s dad
About 150 people every day in the UK are diagnosed with breast cancer, making it the most common form of the disease. It largely affects women, but men also have breast tissue, albeit in much smaller amounts.
So men can get it too?
Around 400 men are diagnosed with breast cancer each year, compared to more than 55,000 women.
Symptoms are similar to those women are told to look out for: a lump or swelling in the breast tissue, liquid leaking from a nipple, any changes to the nipple, or any unusual marks or rash on or around the breast or nipple.
Men are more likely to be diagnosed around 60 to 70, five to ten years later than the average age for women. The risks are similar: older age, exposure to X-rays, and a family history of breast cancer.
US singer Beyonce’s father, Matthew Knowles, recently spoke about his breast cancer diagnosis, which was linked to the same BRCA2 mutation carried by Hollywood star Angelina Jolie.
How to get help
Any of the changes above should be reported to your GP. Treatment might include chemotherapy, radiotherapy, hormone therapy or targeted cancer drugs and surgery.
Migraine is a complex condition caused by changes in the way signals are sent around the brain.
Along with a painful headache, which might be more severe on one side, an attack – which might last up to 72 hours – can also include nausea, vomiting, neck pain and sensitivity to noise, light and smell. And, despite attacks being linked to changes in the female hormone oestrogen, both sexes are affected.
Ben Affleck’s condition isn’t ‘just a headache’
So men can suffer too?
While around one in four women suffer migraines, 12 per cent of men are also affected. The Migraine Trust says this may be an underestimate because fewer men come forward with symptoms and are more likely to dismiss it as ‘just’ a headache.
One of my patients, whose migraines affected his job, was teased at work because ‘migraines are for women’.
In a recent poll by the charity, 84 per cent of men with the condition said it affected their work life, with similar impacts on their general health and social lives. One in five said it left them suicidal.
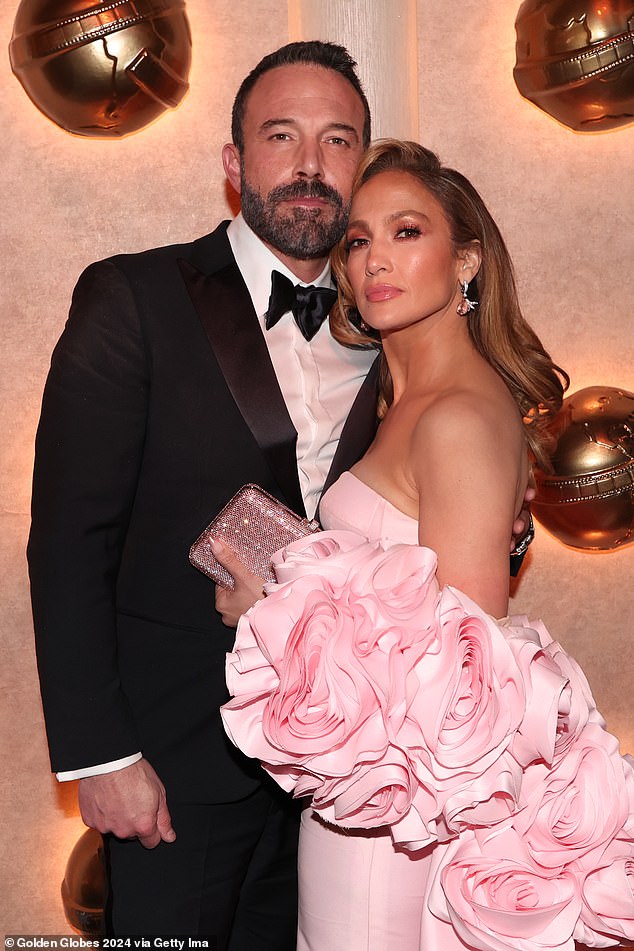
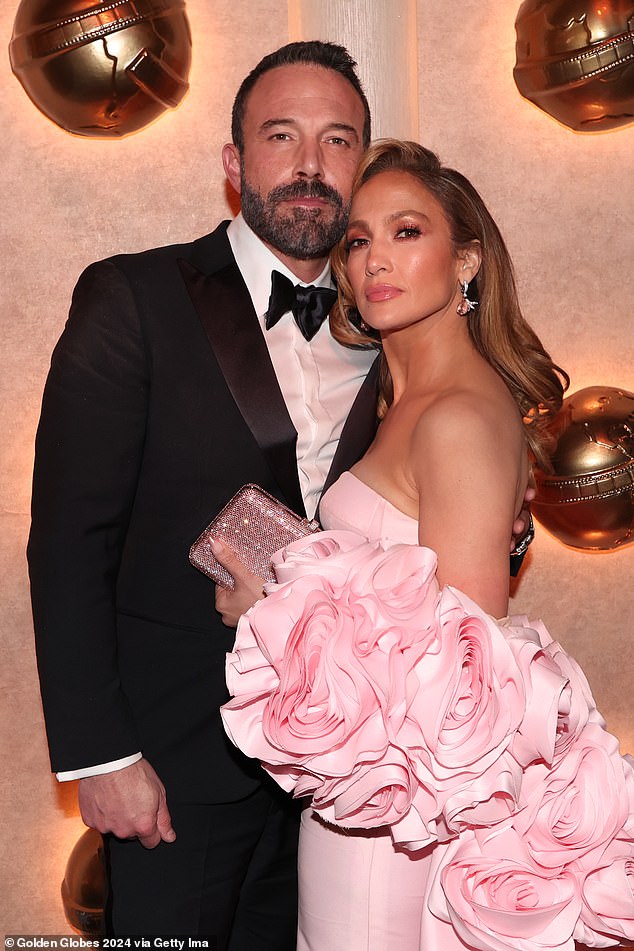
Hollywood star Ben Affleck revealed he was hospitalised with a migraine brought on by stress and lack of sleep while directing his film Gone, Baby, Gone
While it remains unclear what causes migraines, there may be a genetic factor. Common triggers include stress and tiredness, not eating regularly, too much caffeine or not getting enough exercise.
Hollywood star Ben Affleck revealed he was hospitalised with a migraine brought on by stress and lack of sleep while directing his film Gone, Baby, Gone.
How to get help
While taking over-the-counter painkillers such as ibuprofen and paracetamol can help ease symptoms, speak to your GP as it may take a combination of medications to find something that works.
You might be offered a new class of drugs called gepants, which work to block pain signals in the brain. Gepants are safer for those with heart disease – so may be more suitable for some men.
A GP might also recommend lifestyle changes to reduce any migraine triggers, and relaxation techniques.




