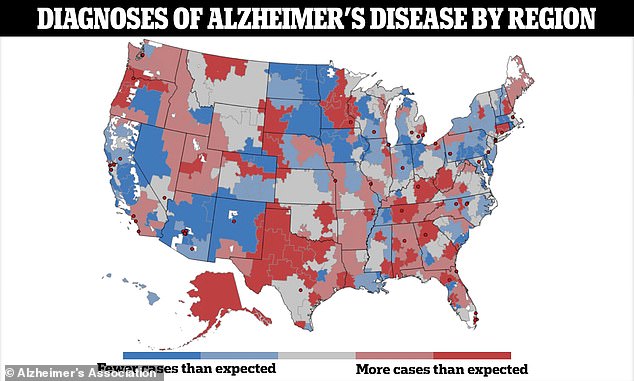
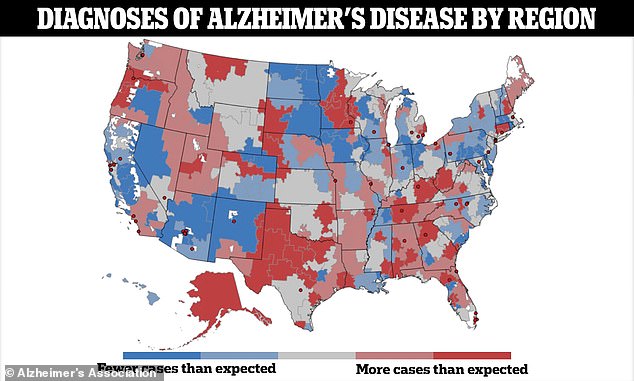
Map shows US Alzheimer’s hotspots by region


New research shows that your chances of developing Alzheimer’s disease depend on your zip code.
Researchers at the University of Michigan found that someone living in a city in the same state is twice as likely to be diagnosed with the memory-destroying disease than someone living a few cities away.
The differences in internal states are likely the result of dementias being missed, the team argued. They blamed variations in screening and testing, irregular health care and education, and differences in people’s willingness to see a doctor.
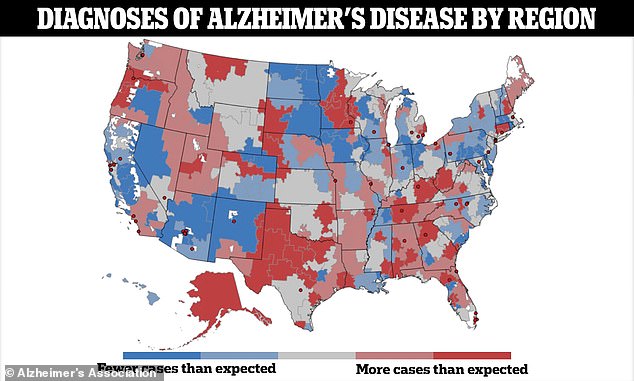
The map shows more than 300 different hospital regions and in each one a ratio that shows the actual number of Alzheimer’s cases compared to the number of cases they would expect. The same person in some areas of the U.S. could be twice as likely to receive a dementia diagnosis than in others.
The overall concentration of Alzheimer’s diagnoses was in the south, along the so-called ‘stroke belt’, where the population has a higher percentage of cardiovascular risk factors.
But even there, there was a patchwork, which the researchers say could reflect varying levels of general health awareness and the signs of illness to look out for.
Dr. Julie Bynum, the UM Health geriatrician and health services researcher who led the study, said: ‘These findings go beyond demographic and population differences in risk and indicate that there are differences at the health system level that can be addressed and remedied.
‘The message is clear: the chance that you will be diagnosed with dementia varies from place to place. This can be due to all kinds of factors, such as the standards that care providers use, the knowledge of the individual patient and the care-seeking behavior.’
This patchwork may reflect populations that are undiagnosed and underserved, as well as differences in the way physicians in different regions practice their work.
For example, physicians in certain regions may be more proactive in diagnosing Alzheimer’s than in other regions.
It could also mean that patients in certain areas are less likely to see a doctor than people in other areas, and therefore go undiagnosed.
The number of Alzheimer’s patients is expected to rise from the current 6.7 million to nearly 13 million by 2050. Addressing the factors that cause disparities between postcode areas could have a huge impact on public health, the team of experts said.
The researchers conducting the study began by analyzing 2018-2019 data from Medicare, the federal health insurance program for seniors 65 and older, to identify cases of Alzheimer’s and other forms of dementia.

The number of Alzheimer’s patients is expected to rise from the current 6.7 million to nearly 13 million in 2050.
Dr Bynum said: ‘The goal today should be to identify people with cognitive problems earlier, but our data show that the younger age group of Medicare enrollees shows the greatest variation.’
“This should be a call for action for communities and health systems to spread knowledge and step up efforts to make services available to people.”
They looked at 306 different regions in the US where hospitals provide highly specialized care to Medicare beneficiaries.
Of the nearly 4.9 million seniors studied, 419,646 had Alzheimer’s disease or another form of dementia. About 143,000 of them were diagnosed in 2019.
They then developed a way to determine the actual number of cases diagnosed in 2019 and compare it to the number they would expect based on statistical models.
This allowed the researchers to see whether more or fewer cases were being identified in certain regions than expected.
They also looked at broader factors, such as the average highest level of education in an area, the rates of obesity and smoking, and how close people live to research centers. These factors could influence how often people are diagnosed.
The results were presented as a ratio between the actual number of diagnoses in a region and the number of diagnoses that would be expected based on the age and health status of a population group.
If the ratio is higher than 1.0, it means that more people are being diagnosed than expected, indicating a high diagnostic intensity.
The prevalence of diagnosed dementia ranged from a minimum of four percent to a maximum of fourteen percent, depending on the region of the hospital referred to. The percentage of new diagnoses of dementia in 2019 ranged from 1.7 percent to 5.4 percent.
The highest rates of Alzheimer’s and dementia were found in the south, along the stroke belt, but there was some variation.
For example, in parts of Mississippi, there were fewer cases than researchers expected, while in central Texas, there were many more cases.
This variation applied to the entire country and the differences between adjacent regions could be very large.
For example, the diagnosis intensity in Portland, Oregon, was 1.2, meaning more diagnoses were made than expected.
But in nearby Bend, Oregon, the diagnosis intensity was 0.8, meaning there were fewer diagnoses than expected.
The researchers did not provide a reason for the differences between documented and expected cases by region, but said it could reflect demographic differences, such as the average age and race of the local population, access to screening and whether someone knows what signs to look for.

The graph above shows the estimated projection of the number of Alzheimer’s patients in the US through 2060.
Those holes weren’t unique to Oregon. They were nationwide on the researchers’ map.
The diagnosis intensity in Gainsville, Florida, was about 1.1. But slightly further south, in more rural Ocala, the diagnosis intensity was 0.9.
And in Providence, Rhode Island, the rate was 0.8. But in Hartford, Connecticut, less than 100 miles to the west, the rate was 1.1.
Their findings were published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association.
It is also possible that some regions may be underestimating Alzheimer’s because people in different parts of the country face barriers to receiving care and getting the correct diagnosis.
The researchers concluded: ‘These findings have important implications for future strategies aimed at improving case detection in these groups.
‘In addition, these findings raise important questions about the extent to which differences in access and care practices may lead to excessive variability in the detection of ADRD.’




