There’s a dangerous wave of patients taking antibiotics… and there’s a very surprising reason why



Telephone GP appointments are causing a worrying rise in antibiotic prescriptions, which could put lives at risk, experts have warned.
The bacteria-fighting drugs are crucial for clearing infections and preventing life-threatening complications. However, the number of difficult-to-treat cases is increasing because the bacteria that cause them are becoming increasingly resistant to the drugs.
Over the past decade, the NHS has made a concerted effort to reduce the number of antibiotic prescriptions given to patients, in order to slow the spread of superbugs.
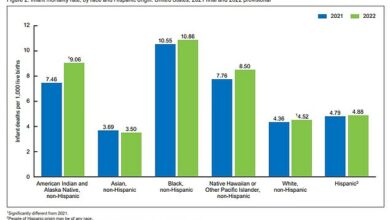
Yet the number is rising again, with almost 37 million prescriptions last year, compared to 36 million in 2022 and 31 million in 2020, official figures show.

Antibiotic prescriptions are increasing again, with almost 37 million last year, compared to 36 million in 2022 and 31 million in 2020
Now experts say fewer face-to-face GP appointments across the NHS could be a major factor behind the rise, as research shows patients seen remotely are significantly more likely to be prescribed antibiotics.
They also warn that the number of antibiotics distributed could be significantly higher than the data suggests because many people turn to private GPs for care – and their prescriptions are not included in the government figures.
“The rise in antibiotic prescriptions is a worrying trend and something must be done to stop it,” said Dr Ryan Hamilton, associate professor of antimicrobials at De Montfort University, Leicester.
‘Remote GP appointments are not the only cause of the increase, but there are good indications that they contribute to this.’
The World Health Organization warns that superbug infections could cause 10 million deaths annually around the world by 2050.
In England, 58,000 people contract an antibiotic-resistant infection every year.
Almost 8,000 people die from such infections in Britain every year. In 2013, in response to the looming crisis, the then Chief Medical Officer, Dame Sally Davies, cracked down on the number of NHS antibiotic prescriptions.
Her focus was mainly on GPs and in 2015 she took the extreme measure of sending warning letters to thousands of GPs deemed to be ‘over-prescribing’ antibiotics.
Dame Sally also accused GPs of bowing to pressure from ‘anxious’ patients and prescribing antibiotics for mild conditions such as coughs and colds, despite the drugs being ineffective against them.
Her efforts were successful, with the number of NHS antibiotic prescriptions falling from 43 million in 2012 to a low of 31 million during the Covid pandemic in 2020.
However, since then the number has increased. Experts say there are several possible reasons.
For example, it has been suggested that as infections become more difficult to treat, more antibiotics are needed to treat them – because a single course of treatment will not be effective.
Nevertheless, a growing number of experts believe that this increase in antibiotic prescriptions is directly related to the decline in in-person appointments since the pandemic.
Since 2019, the annual number of remote GP appointments has increased by around 40 percent, with most taking place by telephone.
Last year, research by NHS England and the charity The Health Foundation concluded that virtual appointments were more likely to result in an antibiotic prescription being written.

An illustration of bacterial transduction, the mechanism that can lead to antimicrobial resistance
The study, published in the journal eClinical Medicine, found that patients with cold and flu symptoms were 25 percent more likely to receive antibiotics if seen remotely, compared to those treated in person.
Experts say remote appointments lead to higher antibiotic use because GPs are ‘more uncertain’ about the diagnosis.
‘When GPs see patients remotely there is more guesswork as they cannot carry out a physical examination,’ says Dr Nisa Aslam, a GP from Watford.
‘If a doctor sees a patient with respiratory symptoms in person, she may check his oxygen levels to make sure his condition is not worsening, or listen to his lungs with a stethoscope for signs of a bacterial infection.
‘But you can’t do this over the telephone. Doctors are therefore more likely to offer antibiotics ‘just in case.’
One patient who knows the danger of drug-resistant infections is Vanessa Carter, 45, from Devon, who contracted the MRSA superbug in hospital after being injured in a car crash in 2004.
‘It was a 10-year battle to clear the MRSA,’ says the mother-of-one, who now works with the charity Antibiotic Research UK as a patient advocate.
‘That’s why it’s so important that we do everything we can to limit the number of antibiotics we take, otherwise more patients will suffer like me.’