What you need to know about IVF, or in vitro fertilization

As the U.S. election approaches, there is national attention focused on a common medical procedure that hopeful parents use to expand their families.
After the Alabama Supreme Court governed (PDF) earlier this year that embryos created through in vitro fertilization have the same legal rights as children, legislators and medical care providers continue to struggle with the fate of reproductive health procedures involving embryos and fertilized eggs. Since 2022, when Roe v. Wade was overturned, it has become less certain whether infertility procedures will remain available under state law.
IVF stands for in vitro fertilization, which is the process of the fertilization of an egg with sperm in a medical laboratory and then implanting the resulting embryo into someone’s uterus, in the hopes that it will develop into a successful pregnancy and baby.
About 2% of all babies born are conceived via IVF each year in the U.S., according to the U.S. Centers for Disease Control and Prevention, and its use has “more than doubled” in the last decade. But despite its growing popularity, IVF remains a complicated procedure, fraught with financial and sometimes emotional burdens for hopeful parents. It also highlights the nuances of human reproduction, whether it’s fertilization in a fallopian tube or conception with a little science.
“I think it’s important for people to understand that as humans we’re not that efficient at reproducing,” said Dr. Asima Ahmad, chief medical officer of Root fertilitywrote in an email to CNET earlier this year. Many embryos created through IVF will not make it to a live birth because they fail to grow further or are unable to implant in the uterus and continue as a pregnancy, for example.
Early embryo losses are also common in “natural” conceptions, even before implantation, but unlike IVF they often go unnoticed and can pass through the body before the pregnancy is even diagnosed.
“There are many things that need to happen correctly for a live birth to occur,” Ahmad said.
Read more: For these personal finance influencers, infertility wasn’t part of the plan
People use IVF for many different reasons. These include medical conditions that make it difficult to conceive naturally, saving childbearing for an age when pregnancy becomes more difficult, and the need for donor eggs or sperm to have a child.
In other cases, people may use IVF or freeze embryos to maintain their fertility if they undergo a medical procedure that may affect their gender, such as cancer treatment, or if they undergo gender confirmation surgery.
How does IVF work?
IVF treatment involves many steps, which is one of the reasons it is so expensive. But it basically involves a process that traditionally takes place in the fallopian tube, giving birth, with additional reproductive assistance from doctors and embryologists as needed by the patient or the doctor performing the IVF procedure.
This is how the process works, according to information from NYU Langone, Johns Hopkins Medicine And Penn Medicine.
Step 1: Collect the eggs
In the month before natural conception, only one egg (sometimes two) is released during ovulation for possible fertilization and pregnancy. But when conception occurs outside the body, you need more eggs to work with, so you will need to undergo an egg retrieval.
In egg retrieval, the person using the eggs for the pregnancy must be given a hormone injection. This allows multiple eggs to mature instead of just one. (Many people who use IVF use their own eggs to conceive, but some patients find an egg donor or even a surrogate to carry the pregnancy.)
To get the mature eggs from the ovaries, you will undergo a process called follicular aspiration, where a very thin needle is passed through the vagina during an ultrasound. The machine sucks out the eggs. You will be given medication to do this. (Fun fact: Human eggs are gigantic (compared to the other cells in our body.)
How often someone needs an egg retrieval depends on a few factors, including the reasons for infertility and age. The number of healthy eggs your body releases decreases with age, so an IVF patient in their 40s, for example, will need more eggs and cycles to have a chance at a successful pregnancy. But some people have higher or lower egg quality and quantity due to their medical history or individual biology, such as sperm or step #2.
Step 2: Collect the sperm
Because much of the sperm production portion of conception occurs outside the body, obtaining sperm for IVF is less medically involved than egg retrieval. Anyone using their sperm during pregnancy will likely be asked not to ejaculate for a few days before collection to ensure a higher sperm count, and most clinics prefer your sample are given at the office.
For those who do not produce sperm with their ejaculation, which contributes to a case of infertility, sperm can sometimes fetched during a minor surgical procedure, which in theory is similar to egg retrieval. Whether you donate sperm before or after egg donation depends on your case and your doctor.
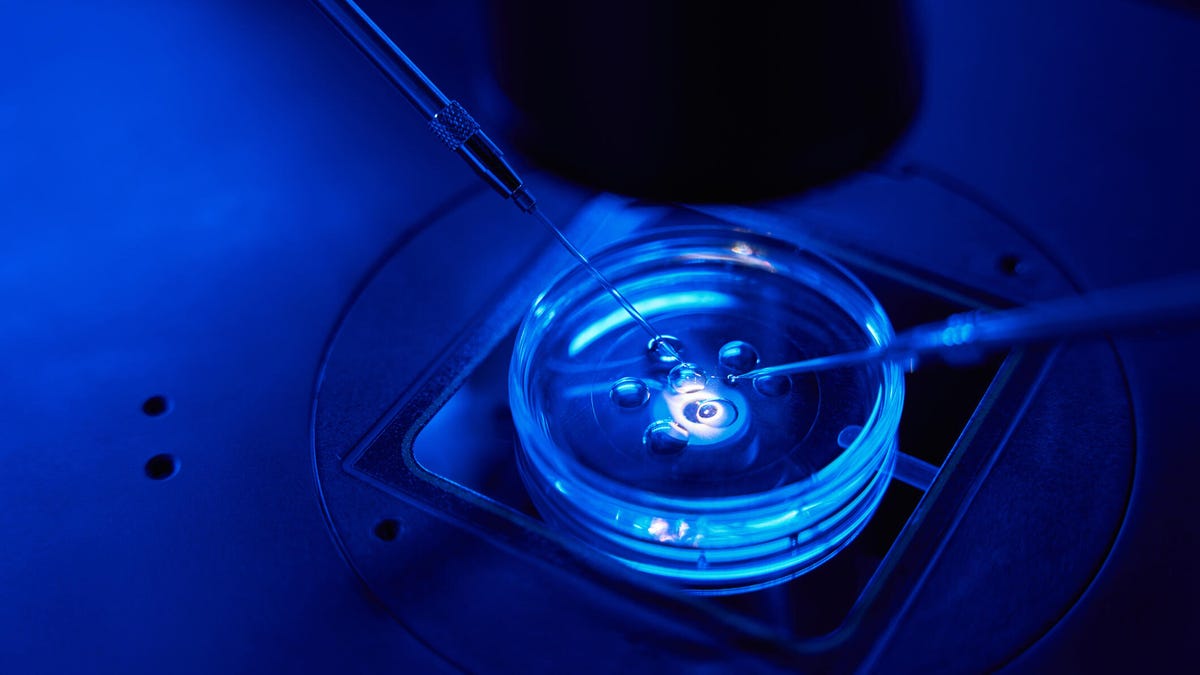
Step 3: Lab fertilizes the egg
Once you have eggs and sperm, the next step in IVF (and how the procedure gets its name) is the fertilization of the egg in a laboratory.
Shortly after the eggs are retrieved, an embryologist will fertilize the eggs, either by allowing a sperm to find its own way to the egg or by injecting a sperm directly into the egg (a process called intracytoplasmic sperm injectionThe method you use depends on your reasons for IVF or your laboratory.
Then everyone waits. It takes about 18 hours to determine if an egg has been successfully fertilized, and then a few more days to see if the embryo is developing properly. In many cases, genetic testing is done on the embryos to determine their health or the likelihood of a baby being born.
Regardless of fertility status, not every fertilized egg will develop into a healthy embryo. Estimates of how many are lost during natural conception seem to varybut half of the fertilized eggs quickly lost after conceptionDuring IVF, these early losses and failed conceptions are literally put under a microscope.
According to Ahmad, the chance of getting pregnant, even at “the most fertile age,” is about 25% to 30% per cycle.
Step 4: Healthy embryo implanted in the uterus
Once an embryo has been selected and has begun to develop, it is transferred into a uterus to allow the pregnancy to proceed normally during a time in the menstrual cycle when the uterine lining can successfully receive the embryo. This is a relatively short procedure where the embryo is released directly into the uterus, passing through the cervix.
After for a whilepatients know whether the embryo is the “come out“process of implanting in the lining of the uterus, which then prompts a person’s body to pregnancy modehopefully resulting in a baby nine months later.
Step 5: Remaining embryos are kept if requested
The Alabama lawsuit from earlier this year revolved around embryos stored by patients at a fertility clinic.
People often have “extra” embryos if they have gone through the first parts of the IVF procedure and were able to get pregnant. If someone wants to have more children in the future, they can keep those embryos frozen in a protective liquid using liquid nitrogen for when they are ready to conceive again. The cost of embryo storage varies by clinic, but can costs at least a few hundred dollars per year, according to an estimate by ReproTech.

Embryos are preserved and frozen using flash freezing with liquid nitrogen to protect the embryos from forming ice crystals that could damage their cells, according to Johns Hopkins Medicine.
People may be left with banked or extra embryos that they don’t know what to do with, have more embryos left over than they originally planned for, are unable to conceive again for medical reasons, or decide not to implant embryos that have been tested to be genetically abnormal or that do not have a good chance of resulting in a healthy pregnancy.
If embryos are not used or frozen, embryos are thrown away as medical wasteor they are transferred into a person’s uterus during a period in the menstrual cycle when pregnancy would not be possible. They can also be donated to science for research, and even to another person.
Whatever the choice, determine the fate of the remaining embryos created during IVF can be difficult for patients for several reasons. The American Society for Reproductive Medicine, an organization that focuses on reproductive science and medical practice, acknowledges the “ethical concerns” that unused embryos pose for patients and the clinics that store them. The ASRM calls patient choice a “core value” of reproductive medicine and that patients’ wishes regarding their embryos “should be respected where practical and within legal limits.” The legal limits on what you can do as a patient depend on state law and individual fertility clinic protocols.
Ahmad says patients generally have some control over how they proceed with their IVF journey, including whether to transfer only “fresh” embryos and not store any (transferring frozen embryos may be recommended by doctors for a variety of reasons, including increased chances of pregnancy), and whether or not to do genetic testing. She notes that some fertility clinics may have individual protocols for freezing all embryos for testing or for other reasons, but IVF choices should involve a risk-benefit discussion between patients and their doctors.
“Ultimately,” Ahmad said, “the goal is to achieve the best possible outcome for the patient.”




