Who is eligible for the mpox jab? As UK confirms first case of deadly new strain that can be transmitted through sex…everything you need to know






The deadly new strain of mpox which has ripped through several African nations has officially reached the UK, health officials revealed yesterday.
The clade 1b mutation, which experts have called ‘ the most dangerous one so far’ kills one in ten of those infected and is believed to be behind a wave of miscarriages.
Officials don’t yet know how the unidentified patient became infected with the strain — though skin-to-skin contact is suspected.
They had travelled back to the UK from a holiday in Africa on an overnight flight on October 21 before developing symptoms a day later.
But all close contacts of the individual have been traced.
The patient has also been transferred to a high-level isolation unit at the Royal Free Hospital in North London — the same facility where imported cases of Ebola were treated in 2015.
So just how worried should we be? Who is most at risk? And what, if anything, should we do to protect ourselves?
Here MailOnline explains everything you need to know.
What is mpox?
Mpox, formerly known as monkeypox, is a viral infection once mainly confined to west and central Africa.
The WHO renamed monkeypox in 2022 to restrain what it called ‘racist and stigmatising language’ surrounding the infection.
Mpox was spread to humans through direct contact with animals such as squirrels, which are known to harbour the virus.
However, it can also be transmitted through very close contact with an infected person, most commonly via sex.
However, mpox isn’t considered a sexually transmitted disease, because it also spreads via other forms of close contact, such as skin-to-skin contact or sharing towels, clothing or bedding with someone who has the virus.
The virus was first discovered when an outbreak of a pox-like disease occurred in monkeys kept for research in 1958, hence the previous name.
The first human case was recorded in 1970 in the Democratic Republic of Congo (DRC) and the infection has been reported in mainly central and western African countries since then.
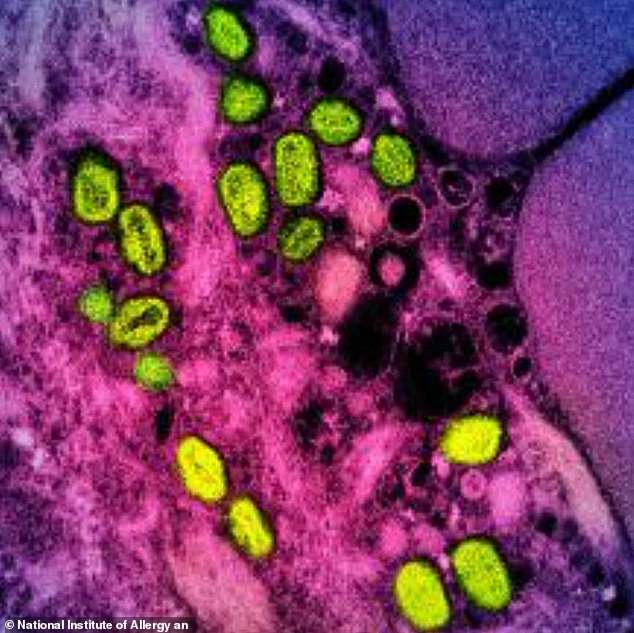
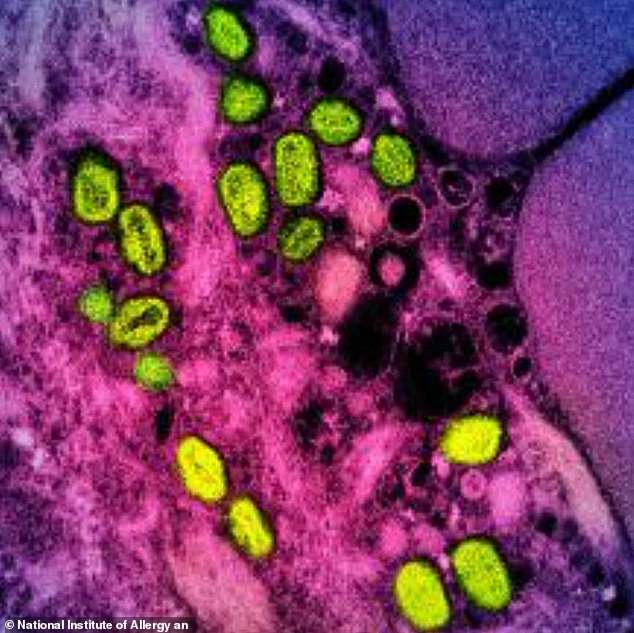
Mpox, formerly known as monkeypox, is a rare viral infection which people usually pick up in the tropical areas of west and central Africa. Pictured, a colorized transmission electron micrograph of monkeypox particles (green) found within an infected cell (pink and purple)
In 2022, an outbreak in Europe and the US that largely affected gay and bisexual men, prompted the World Health Organization (WHO) to declare a public health emergency.
It was the first time mpox had been reported to have primarily spread via sexual contact.
What is the new strain?
Clade 1b is a descendent of the deadly clade 1 strain of mpox and different than the milder version (clade 2) which spread to more than 20 countries, including the UK, in 2022.
Once again, sexual transmission seems to be the primary way clade 1b is spreading.
Researchers believe Clade 1b emerged in September last year, with the first cases found in sex workers in the DRC mining town of Kamituga, around 170 miles from the border with Rwanda.
Clade 1 has historically only been found in people who eat infected bushmeat, with transmission largely confined to the affected household.

It is a far cry from the 2022 outbreak where thousands of cases were recorded, mostly in London
How is it different to other strains?
Clade 1b is considered far deadlier than the clade 2 strain which spread globally in 2022 and primarily hit gay and bisexual men.
Scientists have previously warned the strain was ‘undoubtedly’ the ‘most dangerous one’ yet.
Like Clade 2, Clade 1b causes a severe blister-like rash at the site of the infection.
Symptoms are more severe, with the rash often spreading to the entire body.
It is estimated to kill about 5 per cent of adults who contract it, but the mortality rate rises to one in 10 in children.
In comparison, Clade 2 killed roughly about one in every 500 people that caught it.
But the number of asymptomatic cases or people with minimal symptoms, who could still potentially spread the infection, is also still unknown.
However, experts say fatality rates of clade 1b from central Africa are unlikely to be replicated in developed nations like the UK due to better access to higher quality healthcare.

A woman cares her baby suffering from a severe form of mpox in eastern Democratic Republic of Congo

This map shows the location of mpox cases by UK nation between January 2023 and as of the end of July this year
Where has the mutant form of the virus been found?
Clade 1b has swept through central Africa killing at least 1,000 people, since the outbreak began.
Countries like the Democratic Republic of Congo have been hit especially hard with cases also spotted in Burundi, Rwanda, Uganda, Kenya.
Britain’s case now means it joins countries such as Sweden, Thailand, India and Germany in having cases outside of Africa.
Dr Brian Ferguson, an expert in immunology at the University of Cambridge, said the mpox situation was concerning in part because of how many children it was infecting.
He added: ’40 per cent of cases are in children under 5 years old.
‘As mpox disease is more severe in immunocompromised individuals, it is also a concern that the current outbreak is taking place in a region where HIV prevalence is relatively high but access to antiretroviral drugs is poor.’

After clade 2 sparked alarm among health officials globally in 2022, new infections gradually tapered off amid boosted awareness of the disease and a hurried vaccination program. At the time the UK reported almost 4,000 cases, with NHS England inoculating over 68,000 people against the disease with the smallpox vaccine. Pictured, long lines to receive the vaccine
What do we know about the first UK case?
The unnamed patient had travelled back to the UK from a holiday in Africa on an overnight flight on October 21.
They developed flu-like symptoms 24 hours later, followed by a rash, and attended A&E on October 27 where they were tested for mpox.
Fewer than 10 people are now being contact traced, although authorities are ‘still working’ on the number of people they may have to monitor, the UKHSA said.
No further details on the patient’s condition have been revealed.
But Dr Jake Dunning, a consultant in infectious diseases at the Royal Free, where the patient is being treated, said: ‘Our unit is run by a highly-trained and experienced team of doctors, nurses, therapists and laboratory staff and is specifically designed to ensure the safety of staff and other patients.’
The rest of the NHS hospital is operating as normal.
Officials currently do not suspect the patient was infectious on the flight back from the as yet unnamed African country, they contracted the disease from.
UKHSA said they are currently in conversation with their counterparts in the African nation for contact tracing purposes there and thus are not revealing which exact nation it is.
How deadly is it?
Mpox is usually not serious, with most patients recovering within a few weeks without treatment. Yet, the disease can prove fatal.
Estimates suggest the new mutant strain has a mortality rate of five per cent for adults and 10 per cent for children.
But another worrying aspect was infection in pregnant women was causing an ‘alarming’ number of miscarriages.
Experts have also previously said some cases had even resulted in irreversible sight loss, as well as recurrent whole-body rashes.
Am I at risk?
Officials say they still consider the threat clade 1b poses to the public as ‘low’.
Professor Susan Hopkins, Chief Medical Adviser at UKHSA, said: ‘It is thanks to our surveillance that we have been able to detect this virus.
‘The risk to the UK population remains low, and we are working rapidly to trace close contacts and reduce the risk of any potential spread.
‘In accordance with established protocols, investigations are underway to learn how the individual acquired the infection and to assess whether there are any further associated cases.’
Health and Social Care Secretary Wes Streeting added: ‘The overall risk to the UK population currently remains low and the government is working alongside UKHSA and the NHS to protect the public and prevent transmission.’

The smallpox vaccine works due to the two viruses being closely related. But experts said there wasn’t yet enough evidence to suggest a vaccine would be effective against this new strain
How does it spread and what can you do to protect yourself?
Mpox is not classified a sexually transmitted infection, though it can be passed on by direct contact during sex.
Contagious lesions, through which infections are most likely to be passed on, can appear on any part of the body.
The infection can also be passed on through contact with clothing or linens used by an infected person.
According to the WHO, if someone you know is diagnosed with or has suspected mpox, avoid close contact with them, including sexual contact.
If you have symptoms, seek health advice and self-isolate while you wait to get tested.
Clean and disinfect environments that could have been contaminated with the virus from someone who is infectious.
The US Centers for Disease Control and Prevention (CDC) also says smallpox vaccines and antivirals can be used to treat mpox as well as control it.
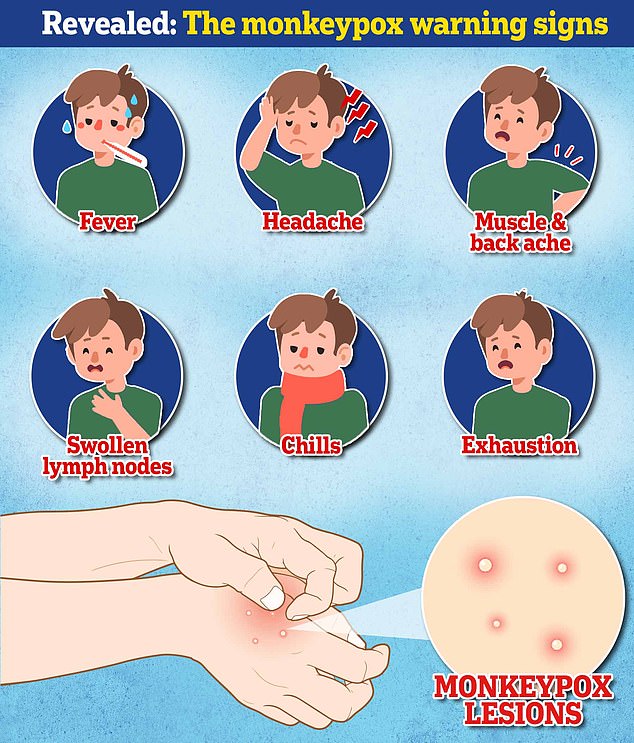
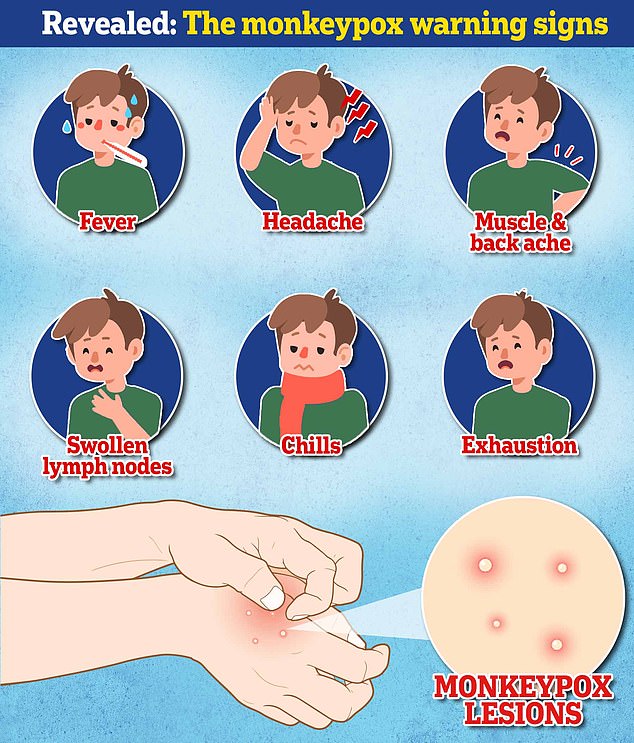
What are the symptoms people should be aware of?
Initially, mpox causes a flu-like illness: fever, headache, sore muscles, back pain, swollen lymph nodes (glands found in the neck, groin or under the arms) and fatigue.
Within one to five days, a rash appears, usually first on the face, then spreading to other parts of the body, including the genitals.
The rash is similar to chickenpox. It starts as raised spots that then turn into small fluid-filled blisters. These blisters turn into scabs, which eventually fall off.
The illness can last up to four weeks, but most cases clear up on their own without any treatment.
During the last outbreak, the UKHSA advised anyone with unusual rashes or lesions on any part of the body – in particular, gay or bisexual men, those who have been in contact with someone who has or might have mpox, and anyone who’s travelled to West Africa in the past three weeks – to contact NHS 111 or phone their local sexual health service.
What happens if someone does test positive in the UK?
If a person is suspected to have monkeypox in the UK, they usually will be given a PCR test – similar to the ones that were used to pick up Covid.
These use swabs taken from the skin and throat.
There are no specific treatments, and the NHS currently says if symptoms are mild, patients may simply be advised to stay at home until they recover.
If the illness is more serious, patients may be offered treatment including antiviral medication — Tecovirimat, which was designed for smallpox, and Cidofovir.
Will the current vaccine work against it?
After clade 2 sparked alarm among health officials globally in 2022, new infections gradually tapered off amid boosted awareness of the disease and a hurried vaccination program.
At the time the UK reported almost 4,000 cases, with NHS England inoculating over 68,000 people against the disease with the smallpox vaccine.
This works due to the two viruses being closely related.
According to the European Centre for Disease Control, data on clade-specific vaccine effectiveness is currently limited.
But public health experts say, because the two strains are 90 per cent similar, they expect the vaccine to work against clade one.
Cases in the Democratic Republic of Congo – the epicentre of the outbreak – are continuing to rise despite the recent rollout of vaccines, which are reportedly taking longer than anticipated to reach badly affected areas.
The campaign launched earlier this month in the country’s hardest hit regions, with jabs donated from international partners including the US, European Union, and Japan.
Limited supply means just 265,000 doses currently available in the country of around 100 million people.