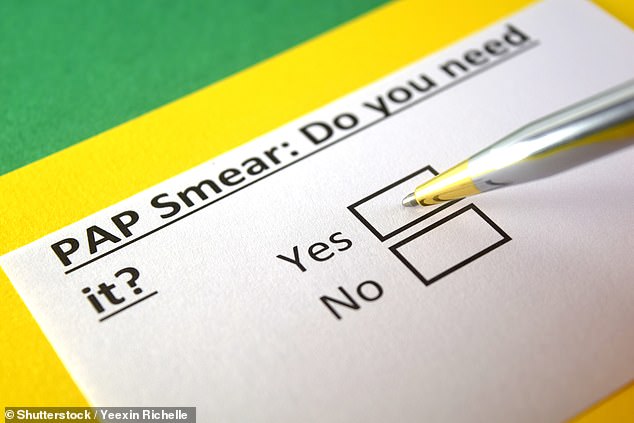
Women want cervical screening done at home to avoid the embarrassment of an intimate test in a clinic, study finds



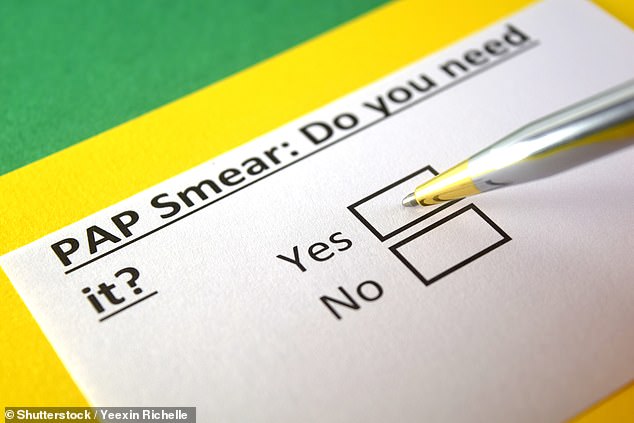

A survey has found that most women are in favor of cervical cancer screening at home to overcome the embarrassment associated with undergoing an intimate test in a clinic.
The NHS offers all women aged 25 to 64 cervical screening tests, previously known as smear tests, every three years. But almost a third of eligible women in England did not take up the offer in 2023, with many saying they did not have enough time or were worried about discomfort and embarrassment.
This test involves taking a sample of cells from the cervix using a vaginal swab – similar to a long cotton swab.
The test is usually carried out by a GP and looks for traces of the human papillomavirus (HPV), a virus linked to cervical cancer. In the UK, there are 3,300 new cases of cervical cancer each year.
Healthwatch England is now calling on NHS officials to offer DIY kits to people who want them, pending ongoing reviews of the tests.

Women want cervical screening to be done at home to avoid the embarrassment of intimate tests in clinics

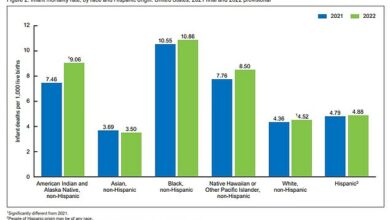
Nearly a third of women eligible for NHS cervical screening tests did not take them up by 2023, with time constraints and concerns about discomfort and embarrassment among the reasons cited
According to the patient watchdog, a poll of 2,400 women found 73 percent would be in favour of home testing if it were made available free of charge by the NHS.
Healthwatch England conducted a survey of women in England aged 24 to 64 who said they were hesitant to accept their next screening offer. Participants said home testing would provide more privacy, avoid inconvenience and could be done at a convenient time.
However, they also cited some drawbacks, including concerns about accuracy and the fact that it was not possible to ask a medical professional whether the test was performed correctly.
In a trial, led by King’s College London and NHS England, patients use a vaginal swab to collect a sample themselves, either at home or in their GP’s office. The swab is then sent to a laboratory for testing. Women diagnosed with HPV were then invited for further testing by a clinician.
Previous analyses suggest that offering self-sampling kits to ‘inadequately screened’ women when they visit their GP could increase uptake in England by around 400,000 a year

In a trial, patients took a smear themselves, either at home or at a GP’s office, and women found to have HPV were invited by a doctor for further testing.
Previous analyses have shown that offering self-sampling kits to women who have been ‘inadequately screened’ when they visit their GP, or sending kits to their home, could increase uptake in England by around 400,000 a year.
NHS England is now investigating how HPV self-screening could be rolled out more widely. A spokesperson said: ‘These findings add to the growing evidence that self-testing can have a positive impact in supporting more women to take part in cervical screening.’
Louise Ansari, chief executive of Healthwatch England, said: ‘Women’s voices must drive improvements in cervical cancer screening and NHS England’s ambition to eliminate cervical cancer by 2040. Support for free home HPV testing represents a significant opportunity to increase the uptake of screening.’
A Department of Health and Social Care spokesperson said: ‘It is vital that access to screening is made as simple and convenient as possible. We are working to explore the possibility of self-collection.’